Our health system is in a state of crisis. This is not a matter of debate: trolley numbers have spiked, waiting lists stretch into years, and medical staff trained at home are leaving in droves due to poor working conditions.
This crisis can be boiled down to two key failings on the part of successive governments: firstly, an extreme depth of fundamental inequality in how patients are treated, differentiated on ability to pay and location; and secondly, the sheer incapacity of the system to deal with even demographic pressures, evidenced particularly in our Emergency Departments and maternity care.
Universal Health Care, not Universal Health Insurance, is the solution.
Sinn Féin is committed to the realisation of a world-class system of universal health care, accessed on the basis of need, free at the point of delivery, and funded by progressive taxation for the Irish state. We believe there is no greater good worth striving for.
Inequality is rife throughout our health system.
| Form of Health Cover (may overlap) | % of population |
|---|---|
| Medical Card | 37% |
| GP Visit Card | 3.5% |
| Private Health Insurance | 45% |
| No cover | 20% |
(Figures from Centre for Health Policy and Management TCD, May 2015)
No two patients are identical; however, some pay more than others for the same care. Families in one part of the country get access to necessary services denied to those in a different HSE region. The less well-off die younger and live less healthy lives. The diminishing minority who can afford private health insurance get to jump the queue.
This is not acceptable. Inability to pay should not deny anyone the opportunity to lead a full, long, healthy life.
We need to increase investment in the health system, not simply to provide more resources and capacity, but to directly challenge and eliminate these structural inequalities.
Investment must prioritise automatic medical cards for children with disabilities, free GP care for all commencing with lower income households, the abolition of prescription charges and extension of free prescription drugs to all, the removal of hospital charges, the rollout of universal dental care, the expansion of ambulance services, and ending two-tier access to public hospital care.
We also advocate exploring the introduction of a new Sinn Féin initiative, the Comhliosta – an integrated hospital waiting list management system, to introduce greater efficiency and fairness across the state and to achieve a sustained reduction in waiting times.
Whether it’s a headline about elderly patients on trolleys in Emergency Departments or children waiting more than a year for speech and language therapy, the common thread across all these stories is the lack of capacity in the system to meet demand.
A lack of capacity means that those in our society who need urgent medical care and attention are left to suffer needlessly as governments dither and institute tax breaks to the better off in society. An unnecessary tax break is of no use to anybody lying on a trolley in a draughty corridor, racked by pain and worry. When we talk about capacity, we are talking about people.
| Health workforce WTEs | ||
|---|---|---|
| August 2008 | 110,899 | |
| August 2015 | 101,917 | |
| Variance | - 8,982 | - 8 % |
(figures from HSE monthly performance reports)
Many young Irish people want to become doctors, nurses, surgeons, or dentists. They go to college and study for years in a system that grows more expensive by the year. When they graduate, they are faced with a health system ravaged by years of austerity, recruitment embargoes and funding cuts imposed by the Fine Gael and Labour Party government and by Fianna Fáil before them. For too many, the choice is plain and emigration is the result.
If we are to stem the flow of doctors, nurses and others from our health system and attract home those that have already left, then we must commence sustained action to address the single biggest factor influencing medical migration – the toxic work environment that currently prevails. Ad hoc, half-hearted recruitment drives will not cut it. To foster and maintain a productive and motivated medical workforce, we must put credible light at the end of the tunnel for staff that things will get better and stay better.
We must guarantee this workforce that the intolerable staff-to-patient ratios will be improved and sufficient resources will be forthcoming that will allow them to actually practice medicine and provide healthcare, not firefight and pen push. This requires a commitment to ambitious multi-annual recruitment targets, with revenue allocated to back these up.
In a term of government, Sinn Féin proposes to recruit more than 6,600 doctors, nurses, dentists, vital administrators and allied health professionals to reinforce the frontline of our health system.
There is no shying away from the commitment that this remedial work will involve. Building adequate capacity across our health system and eliminating the unequal barriers to access will require significant and sustained public investment. It is also difficult to gauge the exact costing involved due to the complex nature of both staffing and treatment costs.
We have endeavoured throughout this document to develop evidence-based costings, but it must be noted that the outcome of negotiations on public sector pay, the terms of service delivery contracts and negotiations with the pharmaceutical industry would impact greatly on the cost of individual measures into the future.
Our costing development work was further frustrated by the staggering deficit of data held centrally by either the Department of Health or the HSE. On a number of occasions, they simply would not, or could not, provide the basic data required to determine what we are currently delivering for our spending. This in itself is of serious concern.
It is, however, undeniable that our public health system continues to suffer acute and chronic underfunding. The annual deficits run up across the system every year, alongside lengthening waiting lists and numbers of patients on trolleys, are a testament to the failure of successive governments to allocate adequate funds.
Sinn Féin is committed to investing what it takes to deliver our vision for the health of the Irish people. And it is possible, despite the aforementioned obstacles, to estimate the additional funds that will be required in the years ahead by examining the macro domestic and international picture.
At 8.1% of GDP (figure relates to 2012, which is the most recent year available from the OECD) our total expenditure on health as a portion of GDP is lower than the OECD average of 8.9%. However, our overall per capita spend, the sum of state-spending and private spending per person, at $3,663 is higher than the OECD average of $3,453. This is despite our comparatively younger population. Yet we do not see any benefit from this, with the number of doctors and hospital beds per resident lower than that of our European neighbours. This is likely because the proportion of our total health spend that comes from private spending by members of the public – including out-of-pocket spending (the money spent by individuals on healthcare, including GP visits and charges for medicines) and private health insurance – relative to public spending is greater than average. It is significantly greater than in countries with the type of health systems we should aspire to build.
The current proportions in the spread of health funding across public spending, private health insurance, and out-of-pocket charges drives inefficiency – as a nation we are literally getting less for more.
The current heavy reliance on private health insurance and out-of-pocket charges is also an inherently regressive policy choice.
For individuals earning a respective wage of €17,000, €35,000, and €65,000, having to pay €144 out of pocket for drugs (which is the maximum monthly spend on drugs before the Drugs Payment Scheme kicks in) accounts for 10%, 5% and less than 3% of their income, respectively. Likewise for the same low, middle and high income groups, the purchase of an average private health insurance premium at €1,200 takes up 7%, 3.4% and 1.8% of their income, respectively.
Due to the fact that the money spent on health ultimately comes from household budgets, the question for policy makers to address is this: what is the optimal way for the money to get from these households to the healthcare provider?
In Sinn Féin’s view, the most effective, equitable, and efficient way to do this is through progressive taxation. In order to deliver universal healthcare we need to increase capacity in the system and progressively replace private spending by members of the public with public spending.
Over the lifetime of the next government we have set out a year-on-year plan to move from a two-tier public-private system towards a universal healthcare system, free at the point of delivery and where access is based on need alone.
The implementation of this plan will require increasing spending on health by €3.3 billion over the next five years. We will increase the health budget each year by the following amounts cumulatively:
| Year | Amount |
|---|---|
| Year 1 | €794 million |
| Year 2 | €771 million |
| Year 3 | €614 million |
| Year 4 | €584 million |
| Year 5 | €518 million |
The above figures are cumulative. The Department of Finance figures for the period 2017 to 2021 set out a combined net fiscal space of €8.6 billion. In prioritising significant and targeted investment in the health service Sinn Féin will allocate €3.3 billion for health from the overall fiscal space for this period. This provision is in addition to a 2%-3% annual funding increase to accommodate demographic pressures.
By progressively replacing private spending by members of the public with public spending, allied with better stewarding of spending, we can achieve much greater efficiency and fairness. We can deliver more for the same.
People would be better off under Sinn Féin’s funding model, not only in terms of the tangible benefits for their health, but in their pockets also. Medical card holders would save up to €25 per month from the abolition of prescription charges and everybody else will save up to €144 per month from the introduction of free prescription drugs. Non-medical card holders will save €100 per A&E visit and up to €750 per year of inpatient charges. Annually expanding numbers will save €50-€60 per GP visit, with free GP care for all reached in the second term of government. Up to 45% of the population will save an average of €1,200 on private health insurance premiums they are currently paying out of fear, as we transform the public health system into the system of choice.
This document identifies the priority actions required to tackle inequality in the provision of health services. It details a five-year programme of investment in the capacity of our health system and in so doing presents a plan to transform our public health system into the system of choice for patients and staff alike.
The document also spells out how we would pay for this, making it the only credible plan for our health system produced by any political party.
The document is structured in three parts – Equality, Capacity, and Funding. Each section provides an analysis of current provision followed by proposals, including estimates as to their cost.
Tá ár gcóras sláinte i gcruachás. Ní hábhar díospóireachta é seo; tá ardú tobann ar líon na ndaoine ar thralaithe, tá liostaí feithimh dhá bhliain ann, agus tá foireann leighis ar cuireadh oiliúint orthu sa bhaile ag imeacht ina sluaite mar gheall ar dhroch-choinníollacha oibre.
Tharla ar an ghéarchéim seo mar gheall ar dhá phríomhtheipeanna rialtas i ndiaidh a chéile; ar an gcéad dul síos an-chuid míchothroime ar an dóigh a gcaitear le hothair, bunaithe ar acmhainn chun íoctha agus áit chónaithe, agus ar an dara dul síos, an easpa iomlán cumais sa chóras le brú daonra a láimhseáil, atá ríshoiléir sna Rannóga Éigeandála agus i gcúram máithreachais.
Is é Cúram Sláinte Uilíoch, ní Árachas Sláinte Uilíoch, an réiteach.
Tá Sinn Féin tiomanta do chóras ar ardchaighdeán de chúram sláinte uilíoch a fhíorú, córas atá inrochtana bunaithe ar riachtanas, agus saor nuair a thugtar é, agus maoinithe ag cánachas forchéimnitheach do stát na hÉireann. Creidimid gurb í seo an mhaitheas is tábhachtaí linn.
Tá éagothroime ann go forleathan inár gcóras sláinte.
| An cinéal cumhdaigh shláinte (d’fhéadfadh forluí bheith ann) | % den phobal |
|---|---|
| Cárta Leighis | 37 % |
| Cárta Cuairte Dochtúra Ghinearálta | 3.5 % |
| Árachas Príobháideach Sláinte | 45 % |
| Gan cumhdach ar bith | 20 % |
(Staitisticí ón Lárionad um Pholasaí agus Bainístíocht Shláinte, TCD, Bealtaine 2015)
Ní bhíonn beirt othar mar a gcéanna; ach íocann cuid acu níos mó ná daoine eile don chúram céanna. Bíonn rochtain ag teaghlaigh i gcuid amháin den tír ar na seirbhísí riachtanacha atá séanta orthu siúd i gceantar eile d’Fheidhmeannacht na Seirbhíse Sláinte. Faigheann daoine nach bhfuil chomh maith sin as le daoine eile bás níos óige agus ní bhíonn saol chomh folláin acu. Faigheann an mionlach atá ag dul i laghad a bhfuil sé d’acmhainn acu íoc as árachas príobháideach sláinte an chéad áit sa scuaine.
Níl sé seo inghlactha. Murar féidir le daoine íoc, níor chóir nach mbeadh an deis acu saol fada iomlán sláintiúil a chaitheamh.
Ní mór dúinn tuilleadh infheistíochta a dhéanamh sa chóras sláinte ní amháin chun tuilleadh acmhainní agus cumais a sholáthar, ach chun dul i ngleic go díreach leis an éagothroime sna struchtúir seo.
Ní mór don infheistíocht tús áite a thabhairt do chártaí uathoibríocha leighis do pháistí míchumasacha, cúram dochtúra ghinearálta saor in aisce do chách ag tosú leis na teaghlaigh sin ar na hioncaim is ísle, deireadh le táillí oideas agus drugaí oideas saor in aisce a chur ar fáil do chách, deireadh le táillí otharlainne, cúram fiacla uilíoch a sheoladh, seirbhísí otharlainne a leathnú, agus deireadh a chur le rochtain dhá leibhéal chuig cúram otharlanna poiblí.
Tacaímid freisin le Comhliosta - Córas Comhtháite Bainistíochta le haghaidh Liostaí Feithimh Otharlainne a fhiosrú ionas go mbeidh éifeachtúlacht agus cothromaíocht níos fearr ar fud an stáit, agus laghdú marthanach a bhaint amach maidir le hagaí feithimh.
Is cuma cé acu ceannteideal atá ann faoi othair scothaosta i Rannóga Éigeandála nó leanaí ag fanacht níos mó ná bliana le hagahidh teiripe urlabhra agus cainte, is í an tsraith is coitianta sna scéalta seo ná easpa acmhainne sa chóras leis an éileamh a shásamh.
Mar gheall ar easpa acmhainne is amhlaidh go bhfágtar na daoine inár sochaí a bhfuil cúram leighis ag teastáil uathu go práinneach ag fulaingt, fulaingt nach bhfuil aon ghá léi nuair a bhíonn na rialtais i mbun na moilleadóireachta agus iad ag tabhairt buntáistí cánach do na daoine is rachmasaí sa sochaí. Níl aon úsáid le buntáiste cánach nach bhfuil aon ghá leis do dhuine atá ina luí ar thralaí i ndorchla fuar, agus iad faoin phian agus imní. Agus muid ag caint faoi acmhainn, is ag caint faoi dhaoine atáimid.
| CLanna Lucht Oibre Sláinte | ||
|---|---|---|
| Lúnasa 2008 | 110,899 | |
| Lúnasa 2015 | 101,917 | |
| Difríocht | - 8,982 | - 8 % |
(Staitisticí ó thuairiscí míosúla feidhmíochta FSS)
Is mian le cuid mhór daoine óga in Éirinn bheith ina ndochtúirí, ina n-altraí, ina máinlianna, nó ina bhfiaclóirí, téann siad ar choláiste agus déanann siad staidéar ar feadh na mblianta i gcóras atá ag iarraidh níos costasaí bliain i ndiaidh bliana. Nuair a bhaineann siad céim amach, ní bhíonn rompu ach córas sláinte a bhfuil dochar na mblianta déine déanta air, tá lánchosc ar earcaíocht ann agus tá ciorruithe maoinithe curtha i bhfeidhm ag rialtas Fhine Gael agus an Lucht Oibre agus ag Fianna Fáil rompu. Is í an t-aon rogha a bhíonn ag an iomarca acu ná dul ar imirce.
Má táimid chun chun stop a chur leis an sreabhadh de dhochtúirí, altraí agus eile amach as ár gcóras sláinte, agus iad siúd atá imithe cheana a mhealladh abhaile, caithimid tosú ar ghníomh leanúnach chun tabhairt faoin tosca is mó ar fad a imríonn tionchar ar imirce lucht leighis – an timpeallacht lofa oibre atá i réim faoi láthair.
Ní dhéanfaidh feachtais ad hoc fhuarbhruite earcaíochta an gnó. Chun lucht saothair leighis táirgiúil, spreagtha a chothú agus a choinneáil, caithfimid ábhar inchreidte dóchais a chur ar fáil go mbeidh rudaí níos fearr agus go bhfanfaidh rudaí níos fearr.
Caithfimid a dhearbhú don lucht saothair seo go mbeidh biseach ar na cóimheasa dofhulaingthe agus go mbeidh dóthain acmhainní ag teacht a ligfidh dóibh leigheas a chleachtadh mar is ceart agus cúram sláinte a chur ar fáil, seachas bheith ag plé le hábhar práinneach agus maorlathas. Éilíonn seo gealltanas i leith spriocanna earcaíochta uaillmhianacha ilbhliantúla le hairgead curtha ar fáil le tacú leo.
I dtéarma rialtais, molann Sinn Féin níos mó ná 6,600 dochtúir, altra, fiaclóir, riarthóir ríthábhachtach agus gairmithe sláinte a bhaineann leo a earcú chun túslínte ár gcórais sláinte a neartú.
Ní féidir an gealltanas a bheidh i gceist leis an obair leasúcháin a shéanadh. Chun cumas ceart a thógáil ar fud ár gcórais sláinte, agus na bacanna éagothroma ar rochtain a scrios, beidh infheistíocht shuntasach leanúnach ag teastáil. Tá sé deacair freisin an costas díreach a bheidh i gceist a thomhas mar gheall ar a chasta atá costais foirne agus cóireála.
Tá iarracht déanta againn tríd an doiciméad seo costálacha bunaithe ar fhianaise a fhorbairt, ach is cóir a mheabhrú go mbeidh tionchar an-mhór ar chaibidlí ar phá na hearnála poiblí, téarmaí conarthaí soláthraithe seirbhíse agus le tionscal na cógaisíochta ar chostas bearta ar leith as seo amach.
Cuireadh isteach a thuilleadh ar ár n-obair forbartha costála mar gheall ar an easpa ollmhór sonraí atá ar coinneáil go lárnach ag an Roinn Sláinte agus an FSS. Ar roinnt ócáidí ní chuireadh siad ar fáil sonraí bunúsacha, nó ní bhíodh siad in ann iad a chur ar fáil, atá ag teastáil chun a chinntiú céard atá á chur ar fáil ar son ár gcaiteachais. Is ábhar mór imní seo féin.
Ní féidir a shéanadh, áfach, go bhfuil ár gcóras sláinte poiblí go fóill ag fulaingt easpa ghéar agus fhadbhunaithe maoinithe. Is léiriú iad na heasnaimh rialta a bhíonn sa chóras gach uile bhliain, chomh maith leis na liostaí fada feithimh agus othair ar thralaithe, ar theip rialtais i ndiaidh rialtais cistí cuí a dháileadh.
Tá Sinn Féin tiomanta an méid infheistíochta a theastaíonn a dhéanamh chun ár bhfís do shláinte mhuintir na hÉireann a fhíorú. Agus is féidir, ainneoin na mbacanna réamhráite, a mheas cé mhéad airgead breise a bheidh ag teastáil sna blianta seo amach trí scrúdú a dhéanamh ar chúrsaí ar an mhacraleibhéal, sa bhaile agus go hidirnáisiúnta.
Ag 8.1% de OTI (baineann an figiúr le 2012, an bhliain is déanaí atá ar fáil ó ECFE) tá ár gcaiteachas iomlán ar shláinte mar sciar de OTI níos ísle ná meán ECFE, 8.9%. Ach tá ár gcaiteachas per capita, suim an chaiteachais stáit agus an chaiteachais phríobháidigh in aghaidh an duine, ag $3,663 níos airde ná meán ECFE, $3,453. Seo in ainneoin ár ndaonra a bheith measartha óg. Ach ní fheicimid aon tairbhe uaidh seo, leis an líon dochtúirí agus leapacha ospidéil do gach saoránach níos ísle ná mar atá ag ár gcomharsana san Eoraip. Is dócha go bhfuil seo amhlaidh mar go bhfuil an sciar dár gcaiteachas sláinte ar fad a thagann ó chaiteachas príobháideach ag baill den phobal (lena n-áirítear caiteachas as póca agus árachas sláinte príobháideach) i gcoibhneas le caiteachas poiblí níos mó ná an meán – agus i bhfad níos mó i gcás tíortha leis an gcineál córas sláinte ar chóir dúinn bheith ag iarraidh a thógáil.
Cuireann na sciaranna reatha sa réimse maoinithe sláinte trí chaiteachas poiblí, árachas sláinte príobháideach, agus táillí as póca, cuireann siad neamhéifeachtúlacht chun cinn – mar náisiún is amhlaidh go bhfuilimid ag fáil níos lú ar son níos mó.
Is rogha pholasaí chúlchéimnitheach é freisin bheith i dtuilleamaí árachas sláinte príobháideach agus táillí as póca (an t-airgead a chaitheann daoine aonaracha ar chúram sláinte, lena n-áirítear cuairteanna ar an dochtúir agus táillí cógas). Do dhuine ar €17,000, €35,000, agus €65,000 de thuarastal, má chaithfidh siad €144 a íoc as póca ar dhrugaí (an t-uaschaiteachas ar dhrugaí sula dtagann an Scéim Íocaíochta Drugaí i bhfeidhm) is ionann sin agus 10%, 5% agus níos lú ná 3% dá n-ioncam faoi seach. Ar an gcaoi chéanna, má chaithfidh na grúpaí céanna ar ioncam íseal, measartha agus ard préimh árachais sláinte phríobháideach a cheannach ag €1,200, is ionann sin agus 7%, 3.4% agus 1.8% dá n-ioncam faoi seach.
Mar gheall air go dtagann airgead a chaitear ar shláinte ó bhuiséid teaghlaigh sa deireadh, is í an cheist a gcaithfidh lucht ceaptha polasaí tabhairt fúithi ná – conas is fearr an t-airgead a thabhairt ó na teaghlaigh seo go dti an soláthraí cúraim sláinte?
Is é tuairim Shinn Féin gurb é an chaoi is éifeachtaí, is cothromaí agus is éifeachtúla le seo a dheanamh ná trí cháin chéimnitheach. Le cúram sláinte uilíoch a chur ar fáil caithfimid cumas a mhéadú sa chóras agus caiteachas poiblí a chur go céimnitheach in áit caiteachas ag baill an phobail Thar shaolré an chéad rialtais eile tá leagtha amach againn plean bliain ar bhliain le bogadh ó chóras sláinte ar dhá leibhéal i dtreo córas cúraim sláinte uilíoch, atá saor ag an bpointe seachadta agus mar a bhfuil rochtain bunaithe ar riachtanas amháin.
Beidh €3.3 billiún ag teastáil leis an bplean seo a chur i bhfeidhm thar na cúig bliana seo romhainn. Méadóimid an buiséad sláinte gach bliain de réir na méideanna seo a leanas go carnach:
| Bliain | Méid |
|---|---|
| Bliain 1 | €794 million |
| Bliain 2 | €771 million |
| Bliain 3 | €614 million |
| Bliain 4 | €584 million |
| Bliain 5 | €518 million |
Tá na figiúirí seo thuas carnach. Leagann figiúirí na Roinne Airgeadais don tréimhse 2017 go 2021 amach €8.6bn de spás fioscach. Agus tosaíocht á déanamh d’infheistíocht shuntasach agus spriocdhírithe sa tseirbhís sláinte, dáilfidh Sinn Féin €3.3bn don tsláinte ón spás fioscadh ar fad don tréimhse seo.
Tá an fhoráil seo mar bhreis ar mhéadú bliantúil maoinithe de 2-3% le freastal a dhéanamh ar bhrú déimeagrafach.
Trí chaiteachas poiblí a chur go céimnitheach in áit caiteachas príobháideach ag baill den phobal, agus trí mhaoirseacht níos fearr ar chaiteachas, is féidir linn i bhfad níos mó éifeachtúlachta agus cothromaíochta a bhaint amach. Is féidir linn níos mó a chur ar fáil ar son an mhéid chéanna.
Bheadh daoine níos fearr as faoi mhúnla maoinithe Shinn Féin, ní hamháin a fhad is a bhaineann sé le sochair inbhraite dá sláinte, ach ina bpócaí chomh maith. Shábhálfadh daoine a bhfuil cárta leighis acu suas le €25 sa mhí mar gheall ar tháillí oidis a bheith curtha ar ceal agus shábhálfadh gach duine eile suas le €144 sa mhí mar gheall ar dhrugaí oidis saor in aisce a thabhairt isteach. Sábhálfaidh daoine nach bhfuil cárta leighis acu €100 ar gach cuairt ar aonad timpistí agus éigeadála agus suas le €750 sa bhliain ar tháillí mar othair chónaitheacha. Beidh líon méadaitheach daoine ag sábháil €50-€60 ar gach cuairt ar dhochtúir le cúram dochtúra saor in aisce do gach duine bainte amach sa dara téarma den rialtas. Sábhálfaidh suas le 45% den daonra ar an meán €1,200 ar phréimheanna árachais phríobháidigh atá á n-íoc acu le teann eagla, agus sinn ag athrú an chórais phoiblí sláinte ón mbonn aníos go dtí an córas is rogha linn.
Sonraíonn an doiciméad seo na gníomhartha tosaíochta a theastaíonn le dul i ngleic leis an éagothromaíocht i soláthar seirbhísí sláinte. Sonraíonn sé clár 5 bliana infheistíochta i gcumas ár gcórais sláinte agus lena linn sin a dhéanamh cuireann sé i láthair plean lenár gcóras sláinte poiblí a athrú ó bhonn go dtí an córas is rogha linn d’othair agus do bhaill foirne araon.
Leagann an doiciméad seo amach chomh maith conas a d’íocfaimis as seo, rud a chiallaíonn gurb é seo an t-aon phlean inchreidte dár gcóras sláinte as measc a bhfuil curtha ar fáil ag aon pháirtí polaitiúil.
Tá an doiciméad seo struchtúrtha i dtrí pháirt – Cothromaíocht, Cumas, agus Maoiniú; cuireann gach ceann acu seo ar fáil anailís ar sholáthar reatha le moltaí ina dhiaidh sin lena n-áirítear meastachán ar a gcostas.
An t-uaschaiteachas míosúil a thiteann ar theaghlaigh faoin scéim um íocaíochtaí drugaí a laghdú go hincriminteach agus amach anseo deireadh a chur le táillí cógais ar fad mar chuid de chúram leighis uilíoch ar chostas tuairim is €160 milliún.
Deireadh a chur leis an táille €100 chun Ranna Éigeandála a úsáid agus an táille €75 sa lá ar chúram othair chónaithigh ar chostas €45.2 milliún san iomlán.
Sinn Féin seeks to build in Ireland a truly fair society based firmly on equality – a New Republic that brings to fruition the ideals and aspirations proclaimed 100 years ago at Easter 1916.
As a party committed to equal rights and equal opportunities as guaranteed in the 1916 Proclamation of the Republic, and to cherishing all the children of the nation equally as pledged by that Proclamation, Sinn Féin is duty bound to bring forward policies and programmes that will make those principles a reality in the lives of the people. In this document we present our policy priorities to achieve a system of Universal Healthcare in Ireland.
As Irish Republicans our aspiration to make healthcare a national priority is also in the tradition of the Democratic Programme of the First Dáil Éireann (1919) which states that “it shall be the duty of the Republic to take such measures as will safeguard the health of the people”. And we look to inspirational figures such as Dr. Kathleen Lynn, 1916 veteran and founder of St. Ultan’s Hospital for the children of the poor, who pioneered public health initiatives in the most difficult and conservative of times. In an Irish Republic worthy of the name, access to high quality public services should be a right for all who live on our island. No public service is more important than healthcare and in no service is equality of access and quality of care more vital. It is a matter of life and death.
The continuing inequalities in public health are a direct result of the deep social and economic divisions in our society, with the wealthier sections enjoying better health and speedier access to healthcare compared to the less well off.
The Department of Health itself admits that “there is an uneven distribution of the risk factors associated with many chronic diseases, with the burden borne disproportionately by those in the lower socio-economic groups. People with higher socio-economic positions in society have a greater array of life chances, more opportunities to lead a more fulfilling life and tend to have better health”. (Department of Health website, ‘Healthy Ireland: Health Inequalities’).
This should be intolerable in Ireland in the 21 st century, yet pervasive social and economic inequality, now as in the past, continues to generate poverty and ill-health in Ireland.
The World Health Organisation (WHO) has defined the social determinants of health as “the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels. The social determinants of health are mostly responsible for health inequities – the unfair and avoidable differences in health status seen within and between countries”.
The Rio Declaration endorsed by WHO Member States at the Sixty-fifth World Health Assembly in Geneva, Switzerland, in May 2012, called upon governments to adopt improved governance for health and development, promote participation in policy-making and implementation and further reorient the health sector towards promoting health and reducing health inequities.
WHO states that if health inequities are to be reduced then the social determinants of health and the provision of universal health coverage need to be addressed in an integrated and systematic manner. Sinn Féin adopts a strong rights-based approach to public policy, rooted in progressive principles nationally and internationally, as set out above.
We seek to address the social determinants of health comprehensively and across all our party policies. If inequality is to be addressed then we argue that progressive policies on wealth distribution, employment, decent pay and working conditions, the environment, enterprise and business, agriculture and food, regional and rural development, education, childcare, social welfare and housing – as well as healthcare – must be implemented.
In healthcare our primary goal is a new universal public health system for Ireland that provides care free at the point of delivery, on the basis of need alone, and funded from fair and progressive taxation.
We seek a fundamental reorientation of the health system to adopt a central focus on prevention, health promotion and primary care.
We advocate healthcare as a right and would enshrine the right to healthcare in a future all-Ireland Charter of Rights and a future United Ireland Constitution.
The model of universal healthcare Sinn Féin is working to achieve includes GP and other primary care, including allied health professionals, medicines, dentistry, hospital care and long-term care. Quality of care is essential and must be at the core of the service.
Such a new comprehensive system will not be achieved overnight but a beginning must be made and that requires political will and a fundamental change in the direction of policy, away from the piecemeal, inequitable, semi-privatised and crisis management approach that has perpetuated the many problems in our health service.
The establishment of the Health Service Executive was a bureaucratic change, top heavy with management, and did not address the fundamental inequities and inefficiencies of the health service. Such structural change is worse than useless without real policy change and improved and better targeted resources at all levels of the service, with priority at all times on the front line of service delivery.
The immediate priority must be to improve access to care for all, removing inequality of access based on income or geographic location and reducing waiting times for care. In parallel with this, real and sustainable improvements must be made and reform implemented in a planned and strategic way, as set out in this document, in order to move definitively towards a universal healthcare system.
The measures contained in this document focus on building greater capacity into the system. For example, more hospital staffing and beds, more services in the community and nursing home places to tackle the recurring trolley crisis, which is really a symptom of the shortage of capacity across the wider health system. Our proposals also focus on tackling inequality. For example, a new consultants’ contract and a single integrated waiting list management system to end two-tier access to public hospital care. And these two strands of capacity and equality are very much interrelated. In order to deliver equal access to GPs we will need more GPs.
We propose to eliminate private activity altogether from public hospitals while replacing this revenue stream. We envisage that the significance of private activity in the overall health system will shrink as we remove the subsidies to it, as we expand entitlements to publicly funded care and as we transform the public system into the system of choice. We propose to incrementally reduce and ultimately eliminate health user charges, from GP fees to charges for prescription drugs, etc. – all in a strategic way and as resources allow.
A point will be reached on this road where the available capacity and public finance will mean that the full suite of health services are being extended to everybody without charge and therefore the different health eligibility statuses or card types, i.e. medical card, GP visit card, long-term illness card, will be redundant.
Significant capital investment will be required to deliver a universal system. A capital programme is not set out in this document but, in government, Sinn Féin will carry out a full review on which to base a 20-year capital programme for our health service. Overall, much investment will be required to compensate for years of under-investment by successive governments. The capital investment in health proposed by the government in ‘Building on Recovery: Infrastructure and Capital Investment 2016 – 2021’ is grossly insufficient. Between 2008 and 2013 public capital expenditure on health was cut by 45%. Under the government’s plan capital investment in health will not even recover to its 2008 level by 2021. Demographic change in the intervening years means the gap between what is needed and what the current government proposes to provide is wider still. In our first term in office, Sinn Féin proposes an additional annual investment of one third over and above that proposed by the current government.
Healthcare is very expensive but what value can be placed on our health and on our lives and what greater priority for public policy could there be? There is no greater good than the health of the nation.
A health service, if it is to truly serve all the people, has to be based on social solidarity. There are plenty of examples of countries where this is the case and where health systems work very well and equitably. This can be done in Ireland also. Otherwise we will continue the creeping movement, amid crisis after crisis, towards the privatised model of healthcare that causes such misery for so many, most notably in the United States.
The greatest resource in the health service is the dedication of those people who work in the service. But workers in the health service and the patients who use it are constantly frustrated by the current system. That cycle must be ended.
It is time for change.
Sinn Féin fully intends to lead in building a renewed health service for Ireland. No party or group can do that alone. But together we can all cooperate to truly transform our health system for ourselves and for those who come after us. This document is structured in three cross-cutting parts as follows:
Inequality is rife throughout our health system.
Some pay more than others for the same care. Families in one part of the country get access to necessary services denied to those in a different HSE region. The less well-off die younger and live less healthy lives. The diminishing minority who can afford private health insurance get to jump the queue.
This is not acceptable.
We need to increase investment in the health system, not simply to provide more resources and capacity but to directly challenge and eliminate these structural inequalities.
Outside of waiting lists for specialists, perhaps nowhere is access to health services more unequal than in primary care. In primary care, entitlements are given or denied on the basis of household finances or employment status rather than medical need.
Investment must prioritise free GP care for all and reforming the medical card system. Likewise, it must diminish the burden of the cost of drugs on those who need them.
Medical bills in the form of drugs and prescription charges are hitting those with the greatest need hardest. We need to abolish prescription charges and have a phased lowering of the drugs payment scheme monthly limit, ultimately leading to free drugs for all.
Provision of dental health is grossly inadequate across the state, with spiralling waiting lists for treatment even for children in significant pain.
We must schedule the exclusion of private activity from public hospitals over time with a multi-annual spending commitment to replace the private revenue stream for these hospitals with public money.
There are certain major public health issues which affect the less well-off socio-economic groups the most. These, which include obesity and addiction, must attract priority action and funding.
Ireland is the only EU health system that does not provide universal access to primary care.
Strong and effective primary care is fundamental to overall health system performance and delivers improved public health. There is also evidence that comprehensive primary care is associated with slower rates of growth in healthcare spending.
The Irish Medical Organisation (IMO) has suggested that we spend as low as 2.3% of our health budget on general practice in Ireland, despite 10% being the norm in many other countries. Since 2009, under the Financial Emergency Measures in the Public Interest legislation, €160 million has been removed from general practice.
Rural and deprived urban areas are in danger of being left without doctors in the coming years because these cutbacks have made some GP practices unviable. There are vacancies in many parts of the country and substantial difficulties in attracting GPs.
It is estimated that there are approximately 14 million visits to GPs annually, compared to 6.3 million hospital visits. We need to prioritise GP care and recognise its important role in our overall healthcare delivery system. We must refocus on primary care with the recruitment of more GPs and support staff, rather than simply building centres for doctors who already have premises to work from.
The focus also needs to shift more towards disease prevention and early intervention, alongside the traditional ‘diagnose and treat’ model.
The General Medical Services (GMS) scheme is the formal title of what is more commonly referred to as the medical card and GP visit card system.
The GMS scheme covers a range of services, including:
About 43% of the population, just short of two million people, have access to free GP care under the GMS via a medical card or GP visit card at a cost of €423 million in 2014.
The remainder of the population, some two and a half million people, must pay themselves to see a GP at a rate of approximately €50 per consultation. They must also pay up to €144 per month for drugs, hundreds or even thousands of euro should they need equipment, and they can be refused the services of a public health nurse.
The Fine Gael and Labour Party Government’s commitment to austerity saw children with serious illnesses and disabilities targeted. Their medical cards were withdrawn, causing outrage in communities across Ireland.
The scale of the outcry is evidenced by the sheer volume of newspaper coverage, with the Expert Panel Report on Medical Need for Medical Card Eligibility noting more than 650 articles on the issue of discretionary medical cards in the months of May and June 2014.
The Our Children’s Health campaign was launched in May 2014 by families impacted by illness and disability who have first-hand experience of the struggle to secure and retain medical cards for their children. Its primary aim is:
“to ensure children with serious medical need are no longer subjected to the crude, unfair, lengthy and frustrating means test in order to be considered for a medical card”.
The campaign has condemned the onerous application process, the exclusive focus on ‘financial hardship’ and the failure to take account of medical need and the impact of a serious medical condition on a child and their family. Our Children’s Health has argued:
“We cannot continue to have a situation whereby children with the most serious medical need coming from ordinary families with modest incomes and huge outgoings remain ineligible. This is simply wrong and unjustifiable.”
The government eventually tasked an expert panel to Report on Medical Need for Medical Card Eligibility (Keane Report).
However, it gave the panel self-defeating terms of reference. It asked them to develop a list of medical conditions which should entitle someone to a medical card.
This was always going to be an impossible task. Eligibility assessments for social welfare, education and indeed health supports have all been actively moving away from basing entitlements or access to supports on diagnosis titles, because it has long been recognised that every condition involves a spectrum of need.
The Keane Report ultimately reached the predictable conclusion that it would be neither possible nor ethical to produce a list of medical conditions on which to base automatic entitlement to a medical card. The Report found “a listing approach risks inequity by diagnosis and a further fragmentation of services”.
And so the inappropriate and burdensome full financial audit of the entire household and all its expenses remains the sole route for a seriously ill child or a child with a disability to apply for a medical card.
Despite its fundamentally flawed terms of reference, the panel, which undertook a public consultation, did succeed in cataloguing examples of the hardship to which illness, disability and the current medical card system give rise. From its online public consultation it noted:
“...difficult decisions being made between accessing GP services for their children or another family member to the detriment of their own health; foregoing necessary GP and/or hospital visits due to cost… restricting medication use, again due to cost. Going abroad to source cheaper medications or specialist care not available in Ireland... created logistical, travel and emotional stress for the individual and their family.” “….The sense of worry, anxiety and stress associated with access (or not being able to access) appropriate health care, and financial concerns associated with cost of care and medications were prominent throughout the submissions.”
From the detailed submissions it received from disease association and patient advocacy groups it noted common themes:
“...Medical Cards should be about medical need, and personal financial circumstances should not be taken into account when assessing for a discretionary Medical Card.” “...accessing community-based services without a Medical Card is difficult and paying for necessary aids and appliances is financially burdensome.” “...many people with chronic illnesses who already have Medical Cards are uninclined to take up employment because they may lose their Medical Card on financial grounds. This further increases their dependency on the State and has a detrimental effect on their wellbeing.”
The Keane Report recommended that the development of a more compassionate medical card system, which accommodates those with significant illness and disability, should be used as a “stepping stone” to the implementation of the first phase of free GP care for all, i.e. prioritise people with chronic illness before allocating care on the basis of age.
It recommended the incorporation of a new Strategic Clinical Advisory Group into the Primary Care Reimbursement Service to give guidance and oversight to the operation of a more compassionate system.
This would ensure the accommodation of cases requiring the recognition of the burden of a medical condition over and above financial hardship. To this end, it recommended that this new advisory group develop an assessment framework and operational guidelines for medical assessors and deciding officers.
Sinn Féin believes that the Department of Social Protection’s Domiciliary Care Allowance scheme provides an example of an assessment model on which a new medical card eligibility test could be based, in that it is independent of both financial means and diagnosis titles. Rather, eligibility is based on reaching a threshold of care needs.
On publishing the Keane Report in November 2014, the government unfortunately reaffirmed its determination to continue to base eligibility for medical cards on financial means. It did, however, concede the need for an ‘enhanced assessment process’ to take into account the burden of an illness or a condition and the clinical advisory group recommended by the expert panel was established. Minister for Health, Leo Varadkar TD, stated:
“From now on, wider discretion and greater humanity will be exercised in such cases.”
However, the horror stories of seriously ill children being refused medical cards and the lengths to which distressed parents are being forced to go to apply for medical cards continue.
Government must urgently introduce and implement a schedule for the extension of full medical cards to people with serious illness and disabilities, without a means test.
In its 2011 Programme for Government, the Fine Gael and Labour Party Government promised to extend free GP care to the entire population, commencing with holders of Long-term Illness Cards and then claimants under the High-Tech Drugs Scheme.
This was to be followed by subsidised care for all and finally universal GP care free at the point of use. That is, the original intention was to prioritise medical need in the roll-out of GP care. During their five years in government, none of this was delivered.
The original commitment to those with chronic illness and disability has long since been abandoned by the government, which engaged in a U-turn and opted to commence roll-out instead to the over- seventies and under-sixes.
While any extension towards universal health care is welcome, the government’s plans have come in for significant criticism.
The Society of St. Vincent de Paul criticised the decision to extend care on the basis of age rather than financial means or medical need.
The IMO stated that GP services are overstretched and priority therefore should be given to those most in need.
Sinn Féin believes that a schedule for the roll-out of free GP care must be guided by medical need, available funding, current capacity in the system and the pace at which further capacity can be put in place.
The Report of the Expert Panel on Medical Need for Medical Card Eligibility (2014) noted that “if deficits in the current and predicted numbers of GPs are not corrected, then universal primary care ‘without barriers’ will not become a reality”.
We know there is a shortage of GPs in this state but the extent of this shortage is difficult to precisely determine. Neither the Department of Health, the HSE nor the Medical Council know the exact number of GPs that are actually practicing in the State and this fundamental data deficit makes scheduling the roll-out of free GP care difficult.
OECD data for 2012 indicates that we have 0.72 GPs per 1,000 population, which is around mid-table.
But we include trainees in these figures, which many other countries do not. This means a more realistic figure might be closer to 0.57 per 1,000 and therefore further down the table.
An article published in the Irish Journal of Medical Science in July 2013, titled ‘Getting a handle on the general practice workforce in Ireland’, estimated that we had 2,954 GPs or 0.64 GPs per 1,000. The corresponding number of GPs in Britain is 0.82 per 1,000 and in France is 1.56 per 1,000. Ireland has only 60% of the number of GPs per thousand population compared to Germany or the US, and only about two-thirds the number of most continental European countries.
On 30 April 2015, there were 2,404 GPs contracted to provide services under the GMS scheme but 3,067 GPs were registered with the Medical Council. It has been estimated that 2,800 doctors are actually working as GPs.
There are also regional disparities in the spread of GPs, with many rural areas struggling to attract GPs to practice and some urban areas where GP practices are overstretched.
The 2010 Expert Group on Resource Allocation in the Health Sector found that expensive, pay-as- you-go GP charges deter use of care. The converse of this finding is that their elimination would, by removing the deterrent, result in greater demand for GPs.
According to the CSO (2011) Quarterly National Household Survey (QNHS) on Health Status and Health Services Utilisation, the average number of GP visits made in the previous 12 months by medical card holders was 5.2. This compares with 2.6 for those with Private Health Insurance and 1.9 for those with neither.
This supports the assertion of the 2010 Expert Group that fees deter use.
If those with free GP access are making between two and three times the volume of GP visits compared to those who must pay at the point of use – and this has consistently been shown to be the case across QNHSs – it must be assumed that the extension of universal free GP care to the entire population will increase the total number of GP visits per annum significantly.
It can be argued that, due to their demographic make-up, those who would benefit from the further extension of free GP care may not increase their visits to as high a rate as medical card holders, even with the removal of the financial deterrent. However, the policy trajectory is also to give GPs a greater role in the management of chronic disease and to encourage people to go to a GP at an early stage rather than resorting to the acute hospital system; all of which points towards more GP visits, at least in the shorter term.
Answering this question is not an exact science. The number needed depends on how many we currently have and on population projections, both of which can be inexact. It will also depend on our success in pursuing various other proposals outlined in this document, such as the recruitment of practice nurses and the expansion of the role of pharmacists, both of which have the potential to free up GPs’ time.
A crude indication may be gleaned from the combination of OECD comparisons and visit rates discussed above. Assuming we currently have 2,800 GPs, we would require an additional 1,200 GPs to bring us up to equivalency with the number of GPs per capita in Britain, for example where GP care is free at the point of use. And calculations based on the likely increase in the volume of GP visits suggest that the extension of free GP care to the entire population could increase the total number of GP visits by nearly 50%, which would require, in the absence of measures to free up their time, an additional 1,300 practicing GPs.
The HSE’s own Medical Workforce Planning September 2015 Report on Future Demand for General Practitioners predicted that by 2025 we will be short between 493 and 1,380 GPs, depending on the extent of access to free GP care.
In 2015, 161 students commenced their four-year GP training, while between 100 and 140 GPs leave or retire every year. Sinn Féin is committed to expanding the GP training programme intake, initially to 200. This has the potential to increase the number of GPs qualifying annually by just short of 40 and the full impact of this measure will not be felt until well into a second term of government. The cost of this increase in training numbers has been estimated at €4.29 million in year one, rising to €17.160 annually by year four, to be sustained thereafter.
| Year 1 | Year 2 | Year 3 | Year 4 | Total Annual Cost | |
|---|---|---|---|---|---|
| 1st Year €cost | 4.29million | - | - | - | 4.29 million |
| 2nd Year €cost | 4.29 million | 4.29 million | - | - | 8.58 million |
| 3rd Year €cost | 4.29 million | 4.29 million | 4.29 million | - | 12.87 million |
| 4th Year €cost | 4.29 million | 4.29 million | 4.29 million | 4.29 million | 17.16 million |
Sinn Féin would seek to make the post of GP more attractive, offering salaried positions with scope for research, links with Emergency Departments, and access to diagnostic tests. We believe that salaried GP posts would ultimately prove to be more attractive. Salaried posts would allow GPs to focus on their clinical role, remove the challenges of running what is effectively a small business, and ease the difficulty of getting locums, something that is deterring GPs at present from pursuing the profession.
Over the lifetime of a full term of government we would seek to introduce 200 salaried GP posts, with a focus on rural and deprived urban areas at an estimated cost of €30.385 million (this figure includes the recruitment of 200 medical secretaries to work alongside the salaried GPs).
Certain areas of the country have been unable to attract a full-time GP for up to three years, despite having a lengthy list of medical card patients, forcing the HSE to employ costly locum doctors. Rural areas in particular lack supports and, as a result of government cutbacks to the Rural Practice Allowance, are financially unattractive to anyone considering establishing a GP practice.
The Rural Practice Allowance was previously paid to a GP who held a GMS contract and who lived and practiced in a centre with a population of fewer than 500 people and where there was no town with a population of 1,500 or more within a 4.83-kilometer radius of that centre. The government reduced this allowance from €3.762 million in 2009 to approximately €3.121 million in 2013. In the summer of 2015 the government announced that they would now grant half the allowance to GPs who work in villages, where there is no town with a population of 1,500-plus within a three- to seven-mile radius. The Rural Practice Allowance should be restored in full in year one at an estimated cost of €0.641 million. Sinn Féin would prioritise these rural areas, and also urban areas where GP services are overstretched, in the allocation of our proposed salaried posts.
Further GP capacity could be freed up by expanding the role of pharmacists, as outlined in section 1.2.3 and through the greater deployment of practice nurses.
Practice nurses are an essential part of primary care provision and 1,800 of them currently work with GPs across the State. They are privately employed by GPs and deal with a wide and increasing range of issues, including patient education, wound management, immunisations, well-women care and screening. In conjunction with our proposed salaried GP posts, Sinn Féin would introduce 200 new practice nurses, who would be directly employed by the State at a cost of €9.366 million.
Sinn Féin’s proposals, outlined in the previous section, to extend secure full medical cards to everybody with a serious illness or disability, would ensure that those who need free GP care for medical reasons get it.
As one of our key priorities on the road to universal healthcare, Sinn Féin proposes to extend universal access to free GP care to the remainder of the population on the basis of financial need rather than age. Over two full terms, we propose to extend free GP care at the rate of approximately 230,000 additional people per annum. This would be achieved by raising the financial threshold for GP visit cards. We estimate that this may cost in the region of almost €28 million in the first full year and a similar additional amount each year thereafter.
Estimates as to the cost of extending free GP care vary significantly: e.g. some experts have estimated that the cost of extending care to 6 to 17-year-olds would be between €17 million and €20 million, whereas the Department of Public Expenditure and Reform has estimated this would cost €79 million.
Actual costs will be contingent on the outcome of negotiations between government and GPs, who are paid on the basis of a combination of capitation rates and fee for service payments, all of which can change at each round of negotiations.
The introduction and expansion of salaried posts would also have the potential to impact significantly on costs. The additional cost of extending GP cards would also be mitigated to an extent by resulting reduced expenditure on the tax relief on GP fees.
Entitlements to the care of public health nurses and allied health professionals can hinge on whether an individual has a medical card. In addition to free drugs and GP care, access to these professionals, whose care can be so vital to securing better quality of life, must be included as a component part of the extension of universal healthcare. As resources allow, the benefits associated with the holding of a GP visit card should be expanded to include care by allied health professionals.
With an increasingly ageing population, and one challenged by growing levels of chronic disease, we need innovative ways to deal with the increased demand on our healthcare services.
We currently spend too high a proportion of our health budget on a small number of hospitals. A greater proportion of funding must be refocused on self-care and primary care. Irish people have been shown to have a high incidence of minor ailments that could be treated more easily and cheaply.
There are also many minor ailments currently treated by GPs that could be dealt with by pharmacists. Pharmacists are very accessible health professionals who have a good relationship with their patients and are experts on medications.
International evidence has suggested that as many as one in seven consultations currently performed by GPs could be dealt with by a pharmacist at a lower cost. In Britain, 18% of GPs’ time is spent on minor ailments.
The cost of treating a minor ailment in an Emergency Department is five times greater, and in a GP surgery three times greater, than the same treatment by a pharmacist.
With the introduction of free GP care, we will need to ensure that GPs are consulted for cases that actually require their level of skills.
We have already seen how training pharmacists to vaccinate against the flu in 2013/14 almost doubled the number of patients vaccinated.
Sinn Féin is proposing a pharmacy-based Minor Ailment Scheme.
Research in neighbouring jurisdictions has shown that ten minor ailments – back pain, indigestion, dermatitis, nasal congestion, constipation, migraine, acne, cough, sprains and strains, and headache – accounted for 75% of the cost of minor ailment consultations and 85% of the cost of prescriptions for minor ailments.
Under the scheme, we propose a patient with a medical card with a minor ailment such as back pain, indigestion or headache have the option of being seen by a pharmacist in the local pharmacy. Following a consultation, the pharmacist would supply the patient with the appropriate medicine from the list of medicines that would be approved for supply under the Scheme.
It could be budget neutral to the Exchequer, as at present GMS patients requiring a non-prescription medicine must present at a GP’s surgery to obtain a prescription which, when dispensed, results in a dispensing fee being paid to the pharmacist.
The fees for supplying medicines to patients under the Minor Ailment Scheme would be the same as those paid for dispensing the prescriptions, so the supply of medicine by the pharmacist would carry the same cost to the State. Such a scheme needs to be introduced across the State.
We know that pharmacy-based Minor Ailment Schemes can lead to reduced GP consultations. According to the Irish Pharmaceutical Union the proportion of patients reporting complete resolution of symptoms after such a consultation ranges from 68% to 94%. And a study showed that 86% of people are in favour of pharmacists being allowed to prescribe medication on a Minor Ailment Scheme.
A study by Drury Research in Ireland (November 2004) indicated that over two-thirds (67%) of Irish adults said that their pharmacist, not their GP, is the first port of call for non-serious medical ailments.
It has been estimated that the policy could free up to 750,000 extra GP consultations per year.
The switching of medications from a prescription to a non-prescription basis could also reduce the reliance on GP services.
The Health Products Regulatory Authority oversees the reclassification from both “prescription-only medicine” to “over-the-counter (OTC) in pharmacy” status, and from OTC to “general retail sale”.
The Authority has identified 32 products that could be reclassified. These include topical antifungals, steroid creams and Proton-pump inhibitors (PPIs). PPIs are commonly prescribed medications that reduce gastric acid production. At present, many products available over the counter from a pharmacist in Britain or the North require a prescription here.
In Ireland, there is no structured follow-up on drug compliance or wastage. We propose that pharmacists review a patient’s medication to improve compliance and reduce wastage of medications.
We know that 30%-50% of patients are not taking their medication as prescribed. International evidence suggests that pharmacist interventions in this manner lead to better outcomes for patients and to quantifiable savings.
In Australia, the government provided funding for pharmacists to provide domiciliary medication reviews which resulted in an average net saving of AS$100 (€62.59) per review for each patient. In 2010, a Health Service Executive/Irish Pharmacy Union working group developed a Medicines Use Review (MUR) project involving primary care teams, GPs and pharmacists. An evaluation of the project found that it achieved its objectives. Other countries have found that such reviews can reduce hospital readmission rates for elderly patients by up to 30%.
The cost of the service in Britain is £28 (€38.01) per patient, but it is clear that the cost of not implementing such a service is much higher and there is potential for substantial savings. We aim to roll out a state-wide pilot scheme focusing on patients aged 60 and over; those taking three or more medications; and those with one or more chronic illnesses, such as diabetes, heart disease/high blood pressure, or respiratory diseases such as chronic obstructive pulmonary disease (COPD) or asthma.
Sinn Féin would pilot a Medicines Use Review initiative commencing with 10,000 patients at an estimated cost of €381,000, with a potential saving of €626,000.
The World Health Organisation has estimated that up to 50% of medicines for long-term conditions are not being taken correctly. In the case of diabetes, this can be as high as 78%.
This is not a surprise, considering the finding by the Royal College of General Practitioners that “half of all adults in England find the health advice given to them by doctors and health professionals too complicated – including instructions on how to take medication appropriately”.
Failure to take medicines correctly can have costly consequences. It can be a matter of life or death. A recently published study in the journal Allergy found that, under testing, less than half of parents of children with severe allergies sampled used an EpiPen correctly.
A New Medicines Instruction Service would give additional support to those who have been newly prescribed a medication in order to promote correct adherence. Such a service is now offered in 90% of British pharmacies and following the introduction of the scheme it was calculated that for each patient who receives the service the NHS saves £190 (€264.47).
It was found to reduce the need for Emergency Department visits and hospitalisations and also to reduce the long-term cost of treatment and of other patient supports.
In terms of the cost of the service, the fee in Britain is £24 (€32.58) per patient, which includes an initial consultation and two interventions. We would propose focusing on certain disease categories as a first step before expanding the service State-wide if a review judges its operation successful.
Sinn Féin’s pilot New Medicines Instruction Service would commence with 10,000 patients at a cost of €326,000, with potential savings of €2.65 million.
Sinn Féin would also explore introducing pharmacist prescribing; this could be started in hospital pharmacies by amending the Pharmacy Act.
We would introduce legislation to oblige pharmacies to inform patients of a pharmacist’s dispensing fees, pharmacy services and mark-ups through in-store displays. Pharmacists would be required to use a standard, clearly visible template and provide the patient or the patient’s representative with an itemised receipt following the dispensing of medicines.
In addition to extending entitlements to GP care that is free at the point of use, in the pursuit of universal healthcare we must also incrementally eliminate the burden of the cost of drugs on the individual.
Evidence shows that charges for drugs can lead to higher health costs in the medium to longer term, not to mention the serious impact they can have on the health of those who need medications.
A study published in the International Journal for Equity in Health, which reviewed 23 papers examining the relationship between prescription drug charges and other health expenditures, found that:
“Prescription drug charges are unlikely to lower total health expenditure and may in fact increase spending overall. Although a decline in the use of services that complement prescription drugs (doctor visits) may lead to cost savings, any savings are likely to be outweighed by increased use of the highly resource-intensive services that substitute for prescription drugs (inpatient, emergency and long-term care).”
Prescription charges for medical card holders were originally introduced under the Fianna Fáil/PD Government by Minister for Health Mary Harney TD and were subsequently increased by Fine Gael and the Labour Party, despite pre-election promises to reverse them.
One of the aims of introducing the charge was purportedly to tackle overuse of medicine. The international evidence, however, is clear. Leading international health organisations, including the WHO and the Cochrane Collaboration, have published reviews that suggest that such charges are not beneficial.
The WHO European Health Observatory found that “charges create financial barriers to access, particularly among poorer people and people with chronic conditions”. There are many ways to tackle overuse but a crude tool like prescription charges is not one of them. Other methods are examined in more detail in section 1.2.3 on pharmacies.
At present those with medical cards are liable to pay a prescription charge of €2.50 for each item that is dispensed, up to a maximum of €25 per month, per person or family. This charge is unfair, nothing more than a tax on being sick and in pain.
Sinn Féin would abolish medical card prescription charges entirely over a term of government, at an approximate cost of €120 million.
Under this scheme, individuals and families without a medical card can pay up to €144 per month for approved prescribed drugs, medicines and appliances.
Again, the evidence suggests that this leads to ill-health and further health costs down the line. This overreliance on out-of-pocket payments constitutes a regressive funding model.
For individuals earning a respective annual wage of €17,000, €35,000 and €65,000, having to pay €144 out of pocket for drugs (which is the maximum monthly spend on medications before the Drugs Payment Scheme kicks in) accounts for 10%, 5% and less than 3% of their income, respectively. We would reduce this unequal burden on families by incrementally lowering the monthly limit on spending to zero. In its September 2015 Report for the Department of Health, the ESRI estimated that the total private out-of-pocket expenditure on prescribed medication was €163 million in 2013.
As outlined earlier in this document, flat fees for health services are not just a regressive funding mechanism; they also do harm because they deter the necessary use of healthcare. In government Sinn Féin would abolish the €100 fee at Emergency Departments, A&Es, Casualties, Minor Injury Units and Urgent Care Centres, at an estimated cost of €9.2 million. We also propose to abolish the €75 per day charge for inpatient care, at an estimated cost of €36 million.
During the recession there was a drastic scaling back across the three main fields of publicly funded dental provision – the Dental Treatment Benefit Scheme (DTBS), the Dental Treatment Service Scheme (DTSS) and the Public Dental Service. Under both the DTBS and DTSS dental care is provided by dentists in private practice, who are paid by the State on a fee-per-item basis.
The DTBS offers certain dental treatments to workers and retirees with the requisite PRSI contributions record. Until 2010 the scheme offered a range of preventative and restorative treatments, including an annual oral examination, biannual scale and polish, extended gum cleaning, fillings, extractions, root canal treatment, X-rays, dentures and denture repairs.
From 2010 onwards, the scheme was cut until it now only covers annual oral examination. Total spending on the DTBS was cut by almost 85%, from €70 million to just €11 million.
Before 2010 the DTSS provided a similar range of dental care to medical card holders. But since then Fine Gael and Labour have eliminated most of the preventative and early diagnostic provisions, including biannual scale and polish, extended gum cleaning and X-rays. Fillings were limited to two per annum. Root canal treatment, dentures and denture repair were limited to ‘emergency cases only’. Ironically, ‘tooth extractions’ are the one thing that was not limited.
Total funding for the DTSS was cut from €87.5 million in 2009 to its current budget of €76 million for 2015.
The Public Dental Service (PDS) provides dental care to children and also to adults with special needs. The PDS is staffed by salaried, public sector dentists. The service was intended to offer dental screening and consequent treatment to children in 2nd class, 4th class and again in 6th class. However, it is doubtful whether the PDS was ever resourced sufficiently to undertake its role and since 2008, the number of dentists employed has been slashed from 387 Whole-Time Equivalents (WTEs) to 315 WTEs in May 2015. This is a drop of 19%, despite demand increasing due to rising pupil numbers.
As a result, children in parts of the State, including parts of Dublin, Kildare, Wicklow and Cavan/ Monaghan have not been getting the first two rounds of screening.
In addition, many HSE dental clinics have closed outright. Since 2008, nine dental clinics have closed across Dublin South West/Kildare West/Wicklow, leaving just 12. Further clinics have closed in Cork, Cavan/Monaghan, Wicklow/Dublin, and South East/West Wicklow, Dublin South Central, Kerry, and Galway/Roscommon.
Waiting lists for children and adults with special needs requiring general anaesthetic for the purposes of dental treatment are shamefully long. Waiting list data provided by the HSE in July 2015 show that 149 adults with disabilities were waiting in excess of 12 months for necessary dental treatment out of a total waiting list of 748.
The data also show 123 children on the waiting list, 26 of whom had been waiting in excess of six months.
The practical result of this is a forced dependence on painkillers for children and for adults with special needs for prolonged and unacceptable periods.
The HSE only extends orthodontic treatment to the most severe cases, i.e. Grades 5 and 4 on the modified Index of Treatment Need. The types of orthodontic problems that qualify include front teeth that are buried and fail to erupt, multiple missing teeth, very prominent front teeth or severe problems with the bite or jaw development.
For those with a severe need who qualify for orthodontic treatment, the wait has been getting longer. Since 2008, the number of Whole-Time Equivalent Orthodontists employed by the HSE has fallen by 8% and the total number on the lists waiting for treatment has risen from 12,978 to 18,025, a staggering increase of 39%.
An English study cited by the HSE found that about one third of all twelve-year-olds could benefit from some degree of orthodontic treatment. Despite this, orthodontic treatment for cosmetic purposes is available here exclusively to those who can afford it.
It should be understood that while such treatment can be described as cosmetic, orthodontic problems often have serious debilitating psychological effects for developing teenagers. Tax relief at the standard rate is available but only after treatment and for many the upfront costs are simply unaffordable. Those families on the lowest incomes may not benefit from the tax relief at all.
The cuts made across the dental schemes have inflicted unnecessary pain and suffering. They have caused an increase in the use of more complicated and expensive emergency treatments as a direct result of the removal of opportunities for prevention and early intervention. This situation has caused significant job losses across the dental sector, forcing many graduate dentists to emigrate, and has undoubtedly led to deterioration in public dental health.
Dental ill-health is closely related to income inequality and all of these cuts have had their greatest impact on low-income families.
Many communities across the State experience lengthy and dangerous delays waiting for ambulances. Isolated rural communities have been underprovided for in many aspects of healthcare and face particular challenges when it comes to ambulances.
The State must guarantee basic levels of care across the country. We recognise that the paramedics in our health service are working under growing pressure, with rising numbers and increasingly complex callouts. The government has failed to support them by providing adequate numbers of staff.
Deeply worrying reports that there were no trained paramedics to work certain catchment areas in Limerick City surfaced in summer 2015. With depleted personnel numbers servicing areas, and some even being left without any emergency cover, this directly increases the risks from serious injury and the potential for deaths.
In 2013, only one in every three cases classified as serious were reached within the target time by the National Ambulance Service (NAS). Failure to meet targets for ECHO and DELTA calls (life threatening emergencies) have been widespread across the state.
The HIQA target requires 80% of ECHO calls for emergency assistance to be dealt with within eight minutes. Last year, in total, just 26.6% of such calls were responded to within this time. In some rural areas just 6.6% of calls were responded to within the eight-minute target time.
The National Ambulance Service currently has a policy of bringing all patients to hospital emergency departments. We must investigate the “see and treat” method used in other jurisdictions. This could halve the number of patients who would need to attend Emergency Departments.
‘On-call’ working arrangements, where paramedic staff are ‘on-call’ – usually from their homes – and must make their way to the ambulance station in order to respond to calls, must be stopped entirely. Assessment of system
A recent report by a British consultancy firm held that Ireland cannot meet current target times because of the size and spread of our rural population. It is also true that survival rates are a better measure of the efficacy of ambulances rather than time-based targets.
However, this report must not be used to further disadvantage rural communities, already forced to rely on greatly reduced hospital services. It must also not be used to further reduce the numbers of ambulances. The report suggested that 290 extra staff are needed at a cost of €15 million a year. We recognise that an investment of this order is needed and our proposal below, which would be introduced in our first year in government, would begin to address the ambulance crisis.
Compared to the Six Counties and to Scotland, the number of ambulances and paramedics in this State per head of population is totally inadequate.
The Chairman of the National Ambulance Service Representative Association, speaking to the Joint Oireachtas Committee on Health and Children, reported that:
“Northern Ireland, with a population of 1.7 million, has an ambulance service that employs just fewer than 1,200 staff. It has a range of just over 300 various vehicles deployed from 57 bases across six counties and an annual budget of £62 million (this equates to €78 million). In comparison, Ireland, with a population of 4.6 million, has an ambulance service that employs less than 1,600 staff. It has a range of various vehicles deployed from 87 bases (of which at least 10% are not 24/7) and an annual budget of €137.4 million”.
Queue-jumping occurs in a number of ways, the most objectionable of which involves private activity in public hospitals enabled by publicly employed consultants on Type B contracts.
There have been recent improvements in equality of access to public hospitals, for example, the introduction of a common waiting list for outpatient diagnostics and treatment. However, it remains the case that those paying privately can access that all-important first consultation with a specialist in a public hospital many times faster than a public patient, regardless of medical need. It is only after this that a patient moves on to a waiting list for treatment.
The government’s ever-extending and often exceeded target maximum timeframe for public patients to wait for this first outpatient appointment is 18 months. Yet private patients can access the same consultant in a matter of weeks, significantly shrinking their overall waiting time for treatment.
Previous waiting list initiatives and injections of cash to the system had a localised or short-term effect but failed to challenge the structural inequality. This cannot be allowed to continue.
We must invest to enhance the capacity of our public hospital system and we must allocate this capacity to patients on the basis of medical need alone. We must eliminate the public/private status differentiation of patients in our public hospitals.
Unacceptable waiting lists persist despite annual spending overruns in the acute hospital sector. Our acute hospital system is undeniably underfunded.
| 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|
| €125 million | €279 million | €70 million | €284 million |
| Acute Service Division | Approved Allocation €'000 | YTD Actual €'000 | YTD Plan €'000 | YTD Variance €'000 | % Var Act v Tar €'000 |
|---|---|---|---|---|---|
| RCSI Dublin North East | 610,722 | 268,779 | 254,428 | 14,351 | 6% |
| Dublin Midlands | 751,491 | 325,583 | 310,858 | 14,725 | 5% |
| Ireland East | 785,137 | 343,742 | 328,912 | 14,830 | 5% |
| South / South West | 692,043 | 294,470 | 286,939 | 7,530 | 3% |
| Saolta University Health Care | 636,218 | 281,722 | 264,523 | 17,199 | 7% |
| UL Hospitals | 257,390 | 108,210 | 106,671 | 1,539 | 1% |
| National Children's Hospital | 221,156 | 94,611 | 92,228 | 2,383 | 3% |
| Regional & National Services | 46,859 | 9,324 | 6,023 | 3,301 | 55% |
| Total | 4,001,016 | 1,726,442 | 1,650,584 | 75,858 | 5% |
Sinn Féin would increase funding for acute public hospitals by €238 million over five years. This is separate to the specific recruitment proposals outlined in the document and over and above increases to cover demographic pressures.
Sinn Féin would explore the feasibility of a new model to maximise the capacity of the public hospital system and introduce fairness and strategic management across all waiting lists. It would also make some use of existing capacity in the private hospital system in the short term.
The component parts of this model include:
An end to the special treatment of private patients in public hospitals by incrementally eliminating private activity and replacing the revenue lost with increased public funding to their Core Activity Budgets during a term of government.
According to the 2015 HSE Financial Statements, in 2014 the statutory public hospital sector got €298 million from private patients. This figure does not include the voluntary hospitals and no figure for that sector was provided in response to parliamentary questions tabled by Sinn Féin.
However, the HSE estimated in its 2014 submission to the Consultative Forum on Health Insurance Review Group that “the Private Health Insurance market generates roughly €500 million per annum for the statutory and voluntary hospital system”.
Sinn Féin would make an additional investment of €100 million, rising to €500 million annually, for the core activity budgets of public hospitals to replace the revenue streams from private insurance.
The first three years of this funding increase would be covered by a corresponding incremental reduction of tax relief on private health insurance, on which €355 million is currently expended.The introduction of a new and single Integrated Hospital Waiting List Management System called Comhliosta.
Under the current system, waiting lists for outpatient appointments, diagnostic tests, day case and inpatient procedures vary drastically from one public hospital to the next. Patients do not know where they stand on the list nor at what speed their list is moving relative to that of other hospitals within reasonable travelling distance. People with comparable health concerns can wait very different lengths of time for assessment and treatment depending on what hospital they happen to be initially referred.
We would introduce a version of the integrated IT system used in the Portuguese NHS, which would help to achieve new maximum wait times by actively transferring those on the list from hospitals that are failing to meet the target to hospitals that have the ability to offer the service on time.
The new maximum waiting times should be developed to cover the entire period from referral to the end of the episode, i.e. the time when either a decision is made not to treat or when treatment has happened.
The IT model introduced by the Portuguese, alongside greater investment in public hospitals, has delivered significant and sustained reductions in waiting times for surgery since it was first introduced in 2004.
As described in the 2013 OECD publication, ‘Waiting Time Policies in the Health Sector: What Works?’, over five years waiting lists for surgery have decreased by almost 35%, the median waiting times by almost 63% and variation across providers is also diminishing.
When a registered patient has reached 75% of the maximum waiting time allowed for their treatment a voucher is automatically generated allowing the patient to obtain treatment in a different public or participating private facility – the payment is the same regardless of provider status.
Unlike the former National Treatment Purchase Fund, fees for Comhliosta activity would be centrally determined and set at a rate below that paid for core activity, which must take account of all hospitals’ fixed costs. In Portugal, the additional surgeries conducted via the transfer system cost, on average, 70% of the price paid for basic surgery provision.
Hospitals in Portugal have an incentive to engage in additional transfer activities over and above that contracted in order to attract the 70% funding which comes with them.
Almost 80% of Irish consultants are currently engaged in some form of private patient activity outside of their contracted hours. This shows they have the capacity to carry out more public activity, which would allow us to treat everybody more quickly and on the basis of clinical need alone rather than patient status. Coupled with greater public investment, Comhliosta could do just that.The renegotiation of the Consultants Contract. As outlined in section 2.3, with the express backing of the public via a clear electoral mandate, our renegotiation would seek to achieve public-only contracts covering core activity on a full-time or part-time basis. Contracts would include protected time for teaching and facilities for research and academic collaborations. Further income could also be generated by consultants by undertaking additional activity transferred to them by Comhliosta outside their contracted hours.
The benefits of this approach could be:
Once in government Sinn Féin will fast-track a scoping exercise to establish the feasibility of Comhliosta. If established, Sinn Féin would make a budget of €10 million available to create our own IT system, using the Portuguese system as a model.
Sinn Féin would also allocate a budget, rising to €100 million annually, for Comhliosta transfer activity.
The shortfall in nursing and consultant numbers is as evident across paediatric services as it is across adult services. The additional medical staff to be recruited over a full term of office, outlined in Part 2, addresses the shortage of nurses and doctors, covers both adult and paediatric services.
Sinn Féin fully supports the proposed new National Paediatric Hospital now earmarked for the St. James’s Hospital site in Dublin 8. We also welcome the commitment to establish two Urgent Care Satellite Centres at Tallaght Hospital and at Connolly Hospital in Blanchardstown.
Sinn Féin is aware of concerns raised by parents and groups regarding the site of the new National Children’s Hospital on the St. James’s Hospital campus. However, many of the services envisaged for the hospital can only be provided through co-location with an adult hospital such as St James’s. It is also important not to add to the delays in delivering what is already an overdue project.
Our main aim is that our children have access to state-of-the-art care in a new facility that can deal with the complexity of modern paediatrics.
The development of a new National Children’s Hospital was first proposed as far back as 1993, when a single tertiary paediatric hospital was originally proposed for Dublin, to be built on the same site as an adult hospital.
The three paediatric hospitals in Dublin have been working in three separate locations as a Hospital Group and the plan is to bring them all together as one entity on one site, tri-located with St. James’s Hospital and a new maternity hospital to be added at a later date. If planning permission is granted, the new Children’s Hospital will be fully operational by 2020.
Local Sinn Féin councillors have met with residents from the community around St James’s Hospital to discuss their concerns regarding the management of traffic during the construction of the new hospital and after it becomes operational.
Adequate space for parking must be included in the proposals for both staff and hospital visitors. Sinn Féin representatives will continue to work with local residents to ensure their concerns are listened to and addressed.
The new National Children’s Hospital must deliver the first-class care our children and their families need, while respecting and working with the local community.
There are fundamental problems with the safety and standard of care that patients receive across this State. Patients report feeling rejected and ignored. Investigations into cases of poor care take far too long.
Recommendations made over many years have not been implemented and conflict has arisen between the HSE and HIQA in relation to reports on care in Portlaoise Hospital.
At present, there are few avenues open to patients trying to navigate a confusing and, at times, an unhelpful system. We believe that a Patient Advocacy Agency would be best placed to address these issues.
Such a body needs to be totally independent of the HSE and to have a staff and a budget that is provided by the Department. It would be inappropriate for a body to be an advocate for patients and also be inspecting facilities at the same time; therefore, this should be a separate entity to HIQA.
We would legislate for the establishment of such an agency and allocate an annual operating budget of €3 million.
We believe that HIQA should be able to pursue enforcement of the standards that it sets out and monitors.
This would give HIQA an oversight role to ensure that recommendations from its reports are implemented. It is clear that, at present, while HIQA can make recommendations for improvements, they are often ignored.
This additional responsibility would help ensure that recommendations made in HIQA reports are acted upon, improving the standard of healthcare throughout the State.
A reporting mechanism would be put in place in the HSE and in the private healthcare sector to notify HIQA of all deaths, serious incidents and adverse outcomes that occur.
We recognise that HIQA has a varied and challenging workload in setting standards and monitoring adherence.
It also needs to be adequately supported and resourced to assess standards in the private sector, now under its remit.
In HIQA’s Business Plan for 2015, they state their intention to increase their staffing from 181 to 228 in 2015. That figure will not be achieved by the end of 2015. With new responsibilities, HIQA will require additional staff. We envisage that we would need to increase staff further to take on the additional enforcement responsibility proposed above.
HIQA’s projected budget for 2015 is €19,100,000, including €9,807,000 on Regulation. We would initially increase this by €625,000 to provide for 10 additional staff.
Health policy is too often focused on responding to problems. We must focus on disease prevention and health promotion.
The government’s Healthy Ireland policy is an interdepartmental initiative to promote public health and is largely very positive.
It aims to fulfil the World Health Organisation Europe’s Health 2020 policy to improve the health and wellbeing of citizens but it needs clear targets and goals along with increased funding.
Healthy Ireland was launched in 2013, but progress to date has been slow. By some measurements, Ireland will have the highest level of obesity in Europe by 2030.
The vision of a healthy Ireland, where everyone can enjoy physical and mental health and wellbeing to their full potential, is a powerful one. Sinn Féin fully supports the goals of the framework, including increasing the proportion of people who are healthy at all stages of life and reducing health inequalities.
However, the sections in the framework on so-called reform are not something that we can support, as they are based on Universal Health Insurance, a critique of which is contained in Part III of this document.
The implementation of the framework must also address the root cause of so much inequality – government policy.
Poverty-proofing of legislation must be introduced across the board and would go some way to addressing geographical and income-based inequalities.
The government has presided over a system where life expectancy is much lower in the most deprived geographical areas, where for men it is 73.7 years compared to 78 years in the most affluent areas. We must eliminate this gap. This will also require a redistribution of resources and further investment in primary care.
| Healthy Ireland Expenditure | |
|---|---|
| 2013 | €89,315.07 |
| 2014 | €586,470.90 |
| 2015 | €252,292.02 (to end September 2015) |
In mid-2015, there were only five staff in the Department of Health assigned to work in the Health and Wellbeing Programme, which is coordinating Healthy Ireland.
Obesity was estimated to have cost the State €1.13 billion in 2009. The most recent WHO reports predict that Ireland is heading for a massive increase in rates of obesity and excess weight.
The government must act now to ensure that these predictions do not become reality.
Statistics from the European Childhood Obesity Surveillance Initiative (COSI) in 2012 suggested that the obesity level among Irish children was 20%, but also that the rate was stabilising in some groups. This was not the case, however, among children in the most disadvantaged communities.
The latest COSI report concludes that the prevalence of obesity in primary school children aged nine has stabilised. Worryingly, this was not observed for children attending disadvantaged schools.
Ireland’s level of obesity has doubled over the past 20 years. Currently, two-thirds of adults and one in four children are overweight or obese. One in five adults are physically inactive and only 25% of children meet the guidelines on physical activity. Even worse, trends have been identified by the Irish longitudinal study on ageing, led by Trinity College Dublin, which found that four out of five people aged over 50 years are overweight or obese.
According to the Irish Heart Foundation (IHF), one in ten children aged between 5 and 12 years is overweight and a further one in ten of this age cohort is obese. In total, 22% of children aged between 5 and 12 years are overweight or obese.
In just one year, Ireland’s only dedicated childhood obesity treatment programme, which is located at Temple Street Children’s Hospital in Dublin, experienced a 400% increase in referrals of children under five.
Obesity affects disadvantaged sectors of society disproportionately but it is a problem that we all must face for the good of our own health and to avoid the costs to our health services that come with it.
Of the estimated €1.13 billion annual cost of obesity, 35% or almost €400 million is attributed to direct healthcare costs, with the remaining €728 million made up of indirect costs such as reduced productivity and absenteeism.
Sinn Féin would introduce a 20% tax on sugar-sweetened drinks and we support the proposal of the Irish Heart Foundation that a portion of this should be ring-fenced to establish a Children’s Future Health Fund.
This would promote a healthier future for all Irish children and particularly for those from disadvantaged areas who are disproportionately affected by obesity and food poverty. It has been estimated by a study commissioned by the IHF that this tax would raise €44.5 million.
In March 2004, Ireland became the first State in the world to ban smoking in the workplace.
Sinn Féin has supported measures to introduce standardised or so-called ‘plain packaging’ for cigarettes and measures to protect young people from the dangers of second-hand smoke in cars.
The emergence of e-cigarettes has led to a legislative vacuum around products that pose a threat to health, albeit in a different way to traditional cigarettes. In the absence of verifiable information on the health impact of e-cigarettes, Sinn Féin would introduce legislation to regulate the sale of these products, specifically banning their sale to children and restricting their sale and promotion to designated premises.
We will also monitor and assess the evidence that suggests they might have a role in assisting people to give up cigarettes or at least provide a less unhealthy alternative. Public Health England, an agency of the British Department of Health, found that they were 95% less hazardous than regular cigarettes. Ireland must protect its public health interests in any negotiations on international trade agreements, including those surrounding the Transatlantic Trade and Investment Partnership (TTIP) – a deal which should be scrapped and which, if passed as proposed, could empower the tobacco industry to challenge measures introduced to protect public health.
In line with the proposals of the Irish Cancer Society, Sinn Féin would introduce an annual tobacco tax escalator.
A portion of the revenue raised could be used to provide additional resources for Revenue and An Garda Síochána to tackle trade in the illicit market.
A deeply worrying report published by the Irish Cancer Society suggests that TTIP could have a damaging effect on public health policy in Ireland.
In its proposed form, TTIP includes mechanisms that would allow multinational corporations to bypass the legal systems of specific States and to seek compensation for barriers to trade.
The authors of the Irish Cancer Society report have made two recommendations — that the Investor-State Dispute Settlement (ISDS) mechanism be excluded and that the proposed commercial arbitration body also be excluded.
Sinn Féin supports both of these recommendations and our representatives in the European Parliament have led the Irish opposition to a trade agreement that is fundamentally undemocratic, lacks transparency and is an assault on the public interest.
We have seen how such mechanisms have led to multibillion-euro cases being taken against governments.
Among the public health issues that could be affected in Ireland are plain packaging of tobacco, bans on using chemicals in certain products, access to clinical trial data and even health and safety legislation.
If the agreement was to be introduced, the Irish Government must ensure the exclusion of health services from its remit.
In the first instance, they must demand that ISDS and the Regulatory Cooperation Body (RCB) mechanism are excluded.
Problem drug use is first and foremost a public health issue. The provision of services aimed at reducing the harm caused by drug use and safeguarding the health of drug users must be central to the next drugs strategy. The current strategy is due to expire in 2016.
In the nine years from 2004 to 2012, problem drug use played a role in the deaths of 5,289 people. That is more than one death every single day. The drugs crisis is a national health crisis.
However, despite the lives of so many – predominantly young men – being on the line, funding for the health services vitally needed to save these lives has been severely cut.
According to the Health Research Board, expenditure and allocations directly attributable to drugs programmes decreased from €276 million in 2008 to €242 million in 2012. The Department of Health and HSE budgets specifically shrank from €39.4 million in 2009 to €30.5 million in 2013, a cut of more than one fifth.
Poly-drug use and alcohol are the primary problems that need to be addressed. Figures from the National Drug-Related Deaths Index published in December 2014 show that there were 350 poisoning deaths in 2012 alone.
Alcohol was involved in 36% of these deaths and alcohol alone was responsible for 22% of such deaths, an increase from 17% in 2011.
Despite the stark scale of the nation’s problem with alcohol, the number of people being treated for problem alcohol use is falling.
According to the latest Health Research Board figures, the total number of cases of treatment has fallen two years running, from a peak of 8,604 in 2011, down to 8,336 in 2012 and then to 7,549 in 2013.
Reports by the National Documentation Centre on Drug Use indicate that the falling numbers of people entering treatment for problem drug use is reflective of the reduced resources allocated to service providers.
We must increase funding for services, make better use of existing health service personnel, pursue simple policy changes and introduce new types of intervention that better meet the health needs of a cohort of people whose lives are often chaotic.
In addition to the measures outlined below, Sinn Féin would increase health funding for the delivery of the National Drugs Strategy by allocating an additional €2.4 million in year one, rising to €12 million over 5 years.
Public Health Nurses (PHNs) work closely with families and during the course of their work problem drug use may come to their attention.
PHNs should be encouraged to take on a more proactive role in responding to this, even where this issue was not the original focus of their involvement with the family. This role would involve exploring and facilitating referral to the most appropriate service or intervention.
It would require PHNs to develop a familiarity with the relevant services in their locality; associated guidance and training for this role should be developed.
Aside from the shortage of public funding and consequent lack of availability of residential treatment spaces, there are further factors which can act as a barrier to accessing treatment, particularly for poly-drug users.
These include a requirement to be drug free prior to admission to a residential programme. There is an urgent need for the introduction of Low Threshold Residential Stabilisation Services based on the principle of open access (including by self-referral), no fee and no restriction on drug use at the time of presentation.
The Ana Liffey Drug Project, which is eager to offer such a service in Dublin, has estimated the annual operating costs of a 20-bed unit at €1.7 million, although it is hoping to obtain a premises on a cost- neutral basis.
Sinn Féin fully supports this initiative and in the short term would allocate the €1.7 million required for the Dublin project.
Despite the welcome expansion of the policy focus within the National Drugs Strategy to include alcohol, the extra resources this requires have not been forthcoming and the number of HSE addiction counsellors has fallen to an all-time low.
In year one, Sinn Féin would increase the number of addiction counsellors initially by 10% at a cost of €698,000, which would provide for 12.3 WTE addiction counsellors, as part of the €2.4 million funding increase proposed above.
Where certain prescription drugs are provided on a monthly basis, the risk of overdose or sale onwards of the drugs can be increased. Controls should be introduced to limit the quantity that can be dispensed by pharmacies at one time for certain medications.
We must not cut corners when it comes to protecting the lives of those dependent on methadone. Buprenorphine is an alternative to methadone. While it is more expensive, it has a significantly safer drug profile.
A number of patients are currently receiving this on a trial basis. Sinn Féin would assess the value of this trial and, if the clinical results are favourable, we would ensure that it is extended as an option to those with opiate dependency. This has been estimated to have a total potential cost of €5 million. Prescribing GPs should engage more proactively with their patients when renewing prescriptions, to reduce methadone dependence where possible, including directing patients to appropriate rehabilitation avenues.
In order to reduce the incidence of overdose, reduce harm to the community from discarded needles and expand the opportunities to reach drug users with wider health and social supports, we should examine the introduction of medically supervised injecting centres on a pilot basis.
These centres have been successfully piloted in Australia and elsewhere. They are staffed by a mixture of medical and social care personnel and can prevent deaths from overdose, facilitate earlier engagement with drug treatment, reduce ambulance call-out costs, reduce the transmission of diseases such as HIV and hepatitis C and diminish the incidence of injecting in public spaces.
Sinn Féin would introduce a pilot programme to examine the merits of medically supervised injecting centres and to that end would pass the necessary legislation to enable these facilities to operate.
The running cost of a centre is estimated to be €1.5 million.
Gambling is a serious addiction issue and one that adversely affects thousands of individuals and families. In recent years medical specialists have seen significant increases in the numbers reporting problem gambling, particularly relating to online gambling. Unfortunately, statistics in this area are sorely lacking.
Sinn Féin would carry out a mapping exercise of the services available to those with a gambling problem and commission a survey of problem gambling to ensure that those who have a problem with gambling have access to counselling. The additional addiction counsellor posts proposed earlier would include a number of positions dedicated to gambling addiction. A portion of the revenue raised by Sinn Féin’s proposal to increase the betting shop tax could be directed to this measure.
Sinn Féin is very aware of the devastating impact alcohol misuse and abuse has on individuals, families and communities. Treating alcohol-related injuries and diseases has been previously estimated to cost our healthcare system €1.2 billion a year.
We have repeatedly called for the early introduction of the Public Health (Alcohol) Bill and, subject to scrutiny, will urge its speedy passage through the Oireachtas. The Bill will include measures on minimum unit pricing, health labelling on alcohol products and restriction and regulation of advertising relating to sports, young people and broadcasting.
We are concerned that its publication has been delayed and that there are now doubts about whether it will be passed before the end of this year.
We need to put in place a broad range of measures to reduce alcohol consumption. The overarching policy must be to prioritise education, prevention and treatment measures. We also believe that the sale, display and advertising of alcohol must be addressed.
Sinn Féin previously raised concerns relating to the introduction of minimum unit pricing at the Joint Oireachtas Committee on Health and Children. If price increases are to be used to reduce consumption, we argued that excise duty should be increased and that all extra revenue generated should be ring-fenced for prevention, education and treatment measures. Our arguments aside, we are willing to facilitate the introduction of minimum unit pricing and will eagerly await and carefully analyse the results over an appropriate timeframe. The importance of measures directed at prevention, education and treatment must not be lost in the MUP approach.
There is evidence that levels of alcohol consumption are inversely related to price and particularly so in those sections of society where alcohol does the most damage.
The evidence spans more than 100 international studies and analysis of these suggests that increases in the price of alcohol are associated with decreases in both alcohol consumption and alcohol-related harm.
A review by the University of Sheffield found that Minimum Unit Pricing targets the price of the relatively cheap and high-strength alcohol, which is disproportionately purchased by those drinking more frequently and in larger volumes.
There is clear evidence that the drinks industry deliberately exploits sport to promote alcohol. A study of 6,600 adolescents in four European countries, published in December 2012 by Amphora, an initiative of the European Commission, found that:
“Alcohol-branded sport sponsorship influences alcohol consumption among adolescents. Exposure to sport sponsoring can predict future drinking.”
Mick Loftus, a former GAA President, has pointed out that:
“Sponsorship of sport creates this culture that you cannot enjoy life without a drink, which is wrong and leads to problems like binge drinking. As a doctor and a former coroner, I know first-hand the damage alcohol does. Eighty-eight people a month die in this country due to alcohol-related reasons. If that number of people were dying any other way they would be taking all sorts of action to try and stop it, but instead they are promoting it. If money comes before people, then it’s a sad day.”
We recognise that some sporting organisations currently receive significant revenue from alcohol advertising but this cannot come before the long-term health of our young people. Given the international dimension of some sponsorship deals, we will explore the potential with other jurisdictions of phasing out alcohol sport sponsorship.
Sinn Féin believes healthcare must be developed on an all-Ireland basis. We should move from increased cooperation to ultimately full integration of services on the island, maximising the healthcare benefits for all and achieving greater economies of scale.
The past decade has seen some developments in health cooperation between the Assembly and Leinster House, with a number of exciting joint departmental projects being developed. These include work on shared radiotherapy and paediatric cardiac services; health promotion focusing on alcohol, tobacco and obesity; cancer research; mental health; and suicide prevention.
It is now agreed that Our Lady’s Children’s Hospital at Crumlin, Dublin, pending the construction and commissioning of the new National Paediatric Hospital at St. James’s, will host the single paediatric heart surgical unit on the island. This will eliminate the need for children to travel from the Six Counties to England for more specialised procedures than those available in Belfast.
Overwhelming clinical evidence supports this decision and the numbers to be treated will ensure that skill levels are maintained by all surgical and support staff. Approximately 140 children a year from the North and 400 from the 26 Counties will benefit from this service.
DBS is a neurosurgical treatment for movement disorders in those with Parkinson’s disease or Dystonia. In the 26 Counties, it is currently funded through the treatment abroad scheme, with patients travelling to Britain and Europe. The high cost of travel abroad and accommodation, including accompaniment in most cases, has made this procedure and follow-on visits prohibitive for many.
The provision of an all-island Deep Brain Stimulation Service has been recommended for full rollout in 2016 and will rely on effective collaboration between neurology services in the South and neurosurgery at the Royal Victoria Hospital in Belfast.
The head of planning and performance in the HSE, in a response to a parliamentary question (PQ) submitted by Sinn Féin, stated that this scheme would “deliver efficiencies with respect to reduced duplication of services and will improve patient outcomes through a coordinated multidisciplinary service”.
We believe that this important step, championed by Sinn Féin’s Health spokesperson Caoimhghín Ó Caoláin TD, will provide a valuable and easily accessible service for all who require this treatment.
There are currently plans for radiology services at Altnagelvin Hospital, Derry, including a Radiotherapy Unit that is due to open in Autumn 2016. This will provide services to patients in the north-west of the island, including from the 26 Counties.
Links between Letterkenny Hospital and Altnagelvin Hospital will create a joint cardiology department, the first ever joint cross-border department in this field.
Thirty million euro has been allocated under Interreg IVA to Cooperation and Working Together (CAWT) Partnership for cross-border health and social care initiatives.
More needs to be done to ensure that access to services is increased, health inequalities are reduced and social inclusion is promoted on a cross-border basis.
Maeve McLaughlin MLA has called for an all-Ireland approach to combatting the rare cancer sarcoma. At present many sarcoma patients have to travel abroad for treatment, often at great expense to themselves and their families.
The international literature supports treatment by specialised multi-disciplinary teams in large, high-volume units. We should examine the development of an all-Ireland approach to patients with sarcoma so they can get the best level of care close to home.
Combining our strength in healthcare will allow more to be done, including more specialised treatments and for a lower overall cost, with patients being able to receive treatment closer to home. It is vital both health systems in Ireland work together to prioritise clinical development across the island and to address the challenges facing healthcare provision in both jurisdictions.
A disease is defined as rare if it affects fewer than 5 persons in 10,000. People often have to wait many years for the correct diagnosis and even then their doctors may be unsure how to proceed in terms of the best care pathway. For those affected by rare diseases, co-operation across the island of Ireland, Europe and internationally is especially important. The National Rare Disease Plan 2014- 2018 commits to the establishment of an All-Ireland Network of Rare Disease Registries. The Genetic and Rare Disorders Organisation (GRDO) has described these registries as “crucial building blocks for sound policy on rare disease”. GRDO states:
“Where well-implemented registries exist, there is better understanding of prevalence, impact and the likelihood of developing a treatment for the rare disease in question is increased. Furthermore, the collection of patient data creates better standards of care and dramatically improves patient outcomes and life expectancy.”
The All-Ireland Network of Rare Disease Registries must be developed and it must be properly resourced. The number of consultant geneticists and genetics counsellors employed in the 26-County public health system falls short of the Royal College of Physicians (Britain) recommendation of a minimum of three consultant geneticists per million people and of the Association of Genetic Nurse and Counsellors (Britain) recommendation of one genetic counsellor per 100,000 people. This results in unacceptably long waiting times and must be addressed.
In November 2014, Dr Stephen Thomas of Trinity College Dublin’s Centre for Health Policy and Management said that we have experienced “the biggest proportionate drop in healthcare across Europe… We’ve lost almost 20% of our health funding, and certainly about 11%-12% of our staff.” We have lost almost 2,000 nurses since Fine Gael and Labour came to power, and this follows a massive drop under the preceding Fianna Fáil administration.
We also have some of the lowest numbers of consultants, including the lowest numbers of obstetricians and gynaecologists per 100,000 women across the OECD.
On 6 January 2015, 601 patients were waiting on trolleys across the State, a record high. This represents a total failure by Fine Gael and Labour.
The Taoiseach committed that he would “end the scandal of patients on trolleys” as far back as Fine Gael’s 2007 election campaign.
This year, there were almost 70,000 patients waiting for surgeries such as hip replacements or cataract procedures and a further 402,156 were waiting to be seen by a specialist on an outpatient basis.
The only way to truly tackle the exodus of trained staff across healthcare professions is to improve our healthcare system.
We must ensure that we have adequate numbers of professionals, protect them from exploitation and overwork, and provide the support they need.
We need to combat the exodus to the private sector and overseas. We need to address working conditions, training and career pathways and pay as we transform the system into an attractive work environment.
Certain groups need to be prioritised for recruitment. For example, as explained in Part 1, GP numbers need to increase significantly in parallel with the rollout of a free-to-access GP service for all. We also need to address the trolley crisis. Waiting times for inpatient and outpatient care cannot be brought down significantly if we do not have the healthcare professionals to provide the necessary services.
We need to focus on recruitment of additional consultants and specialist nurses.
A very significant increase in capacity across the system is vital if we are to overcome the current crisis and move towards genuine universal healthcare.
When the current government claims to have increased nursing numbers by 1,000, they neglect to mention that they have overseen an overall drop of almost 2,000 nurses since coming to power.
Together the three parties, Fianna Fáil, Fine Gael and the Labour Party, have presided over the loss of 4,795 nurses between 2007 and 2014.
| Nursing Numbers | |
|---|---|
| 2007 | 39,006 |
| 2011 | 36,783 |
| 2012 | 34,637 |
| 2013 | 33,735 |
| 2014 | 34,211 |
Each year, approximately 1,500 nurses complete their nursing degree programme in the State. This is recognised as the minimum number to maintain nursing numbers at the level required.
However, the government’s strategy to shrink the health workforce via the recruitment embargo and voluntary redundancy programme had a massive impact on nursing numbers.
The declining numbers of nurses has been exacerbated further by the resulting poor working environment. This inhibits efforts to retain and recruit more nurses in a vicious downward spiral.
Any effort to retain existing and recruit further nursing staff will only succeed if a believable financial commitment is made by government to expand health workforce numbers to the level needed to radically reshape the working environment in our health system.
A HSE internal audit from last year shows that one nurse had worked an average 75.47 hours a week in the first six weeks of the year, thereby contravening the European Working Time Directive, while also earning €5,500 in overtime in a single month. This shows the pressure that certain nurses are under. The system is failing to recruit adequate numbers to share growing workloads.
Half-hearted commitments to recruit a meagre fraction of what is needed are doomed to failure. Nurses will only be enticed to remain, and to return, if they are confident that in the years ahead our health system will become a good place to work.
The HSE has initiated a new recruitment campaign that aims to attract 500 nurses and midwives to come to Ireland, focusing mainly on Irish graduates. The HSE will offer a relocation package worth €1,500 including flights, registration and postgraduate course funding. The salary scale is €27,211 to €43,800 with additional pay for shift and differentials.
We know that the NHS is actively recruiting Irish nurses. According to the INMO the NHS is currently offering packages worth up to £3,000 sterling and numerous enticements to Irish nurses to work in Britain.
The ‘yellow pack’ nurse scheme, first announced by government in 2012, whereby newly qualified nurses were being paid up to 20% less for their first three years of work, has been shelved. Sinn Féin condemned this scheme from the outset.
The scheme was supposed to recruit 1,000 nurses but in fact helped to drive the exodus of nursing staff from Ireland. The Irish Nurses and Midwives Organisation (INMO) has stated that approximately 9,000 nurses have left Ireland since 2009. It has been estimated that it costs approximately €100,000 to train an individual nurse.
The HSE employed 39,006 nurses in 2007, its highest ever number. Since then, this figure has fallen progressively, to 34,211 at the end of 2014.
Fewer nurses are caring for ever increasing numbers of patients who are more susceptible to illness and are more frail. Nursing numbers must ultimately return to at least this pre-austerity level if we are to give our people nursing care of adequate quality and give nurses the assurance that they will not be overworked.
To reach this level, we would need to increase the number of nurses by 4,500. Realistically, this cannot be achieved over a single term of office.
Our recruitment efforts need to make clear that we are committed to ensuring we have enough nurses to support the system we wish to build, without imposing an unfair workload on them. In government, Sinn Féin would seek to increase nursing numbers by an additional 500 nurses each and every year over a five-year term, to be followed by further recruitment.
Despite recent modest recruitment efforts, the nursing registration system is hindering progress. There is currently a backlog due to lack of staff and funding in the Nursing and Midwifery Board of Ireland (NMBI).
In summer 2015, 2,016 applications were being processed, with 698 applications in the system for more than a year. The Department of Health has authorised additional resources to aid the NMBI in clearing the backlog but more will be needed to cater for the true scale of recruitment that is required.
We need increased support for further education and regularising nursing and midwifery acting positions. We would continue improving the adaption programme or devise an alternative to it in order to facilitate nurses who have trained abroad to adapt to the Irish system.
Despite the focus of recruitment campaigns overseas, there are large numbers of nursing staff here already on part-time or even zero-hour contracts who would be interested in taking up further hours or full-time posts. We would engage with these qualified nurses at home.
Nurse prescribing is just one example of the opportunities for professional development in which we must invest to maximise the capacity of our health system and to ensure that nursing remains an attractive career option.
Nurse prescribing has been found to be a positive development for patients and for nurses. It was also found, when independently evaluated, to support professional development. Patients and staff were very positive about the experience and found that it reduced waiting times, while also being safe and effective.
At the start of 2015, 1,114 nurses and midwives had been funded by the Office of the Nursing and Midwifery Services Director to undertake education programmes.
There are 177 health service providers supporting the introduction of medicinal product prescribing by nurses and the number of Registered Nurse Prescribers is 767.
We currently have 2,800 consultants. In April 2015, out of the total of 2,947.5 consultant posts, 234.5 were unfilled (8%). Approximately 100 consultants exit the workforce each year, mostly because of retirement, some due to emigration.
Two to three hundred new medical consultants are required to fill vacancies which currently exist and which will arise over the next twelve months.
The Hanley Report 2003 recommended that by 2012 there should be 3,600 consultants. Therefore, the number of approved posts is currently 800 short of the target that was set over 12 years ago. The Strategic Medical Workforce Planning (MWP) Project started in July 2013 aimed to develop a medical workforce planning system by June 2015 with projections for all medical specialties over time. It has not yet concluded its work.
30 June 2015
Type A 520 (a public consultant who does public practice in a public hospital exclusively)
Type B 1566 (a public consultant who can engage in private practice only in a public hospital in which they are employed) [St. Vincent’s University Hospital is currently in dispute with the Health Service Executive over whether consultants employed in public institutions on a Type B contract can engage in practice in an associated or nearby private facility.]
Type B* 289 (a B* contract refers to a public consultant who can practice both in a public hospital and privately offsite.)
Type C 54 (a public consultant who can engage in private practice both in the public hospital in which they are employed and offsite)
Category 1 201
Category 2 166
Other 4
Posts open for recruitment on 16 July 2015 include 62 Type A consultant posts and 169 Type B consultant posts.
In June 2014, the Strategic Review of Medical Training and Career Structure (Mac Craith Report) made 25 recommendations addressing a range of barriers relating to the recruitment and retention of doctors. In 2015, fewer than half (10) of these recommendations are at advanced implementation phase.
The Mac Craith Report should be implemented, but care should be exercised in relation to proposals on contracts and reconfiguration of hospital services, ensuring that the public good and a geographical spread of access to care are retained.
Many consultants choose to work abroad. Difficult working conditions, long working hours, poor support and uncertain career pathways are major issues.
Specific problems raised by training specialists are complicated systems, very high bed utilisation, underfunding of primary care leading to further pressure on hospitals and poor use of information technology.
The level of compliance with the EWTD 48-hour working week was 68% at the end of January 2015. This needs to be fully implemented. One in eight trainees have said they are planning to emigrate post-qualification and a further 25% are undecided. Working conditions are strongly linked to this exodus.
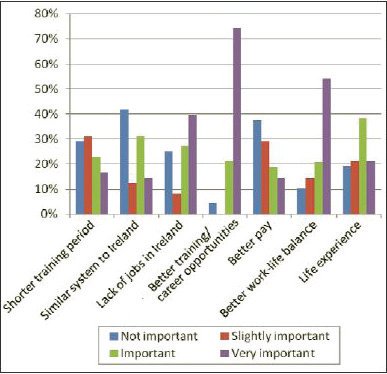
A survey, ‘Diagnosing the Doctors’ Departure: Survey on Sources of Dissatisfaction Among Irish Junior Doctors’, published in 2012, of 522 Irish Non Consultant Hospital Doctors (NCHDs), carried out to establish why so many junior doctors were leaving to seek work abroad, found that the most important reason was better training and career opportunities.
The overall state of the healthcare system, lack of staffing cover, and having to move around the country to various posts were also highlighted.
More recent research by Niamh Humphreys of the Royal College of Surgeons in Ireland and others examining the experiences of various medical professionals, including consultants, NCHDs and nurses who have emigrated, confirmed these motivational factors.
We currently produce enough graduates, but we find it difficult to retain staff. We are heavily reliant on internationally-trained staff who are in turn departing Ireland for similar reasons to their counterparts and the absence of career and training opportunities in particular. Postgraduate opportunities should be more accessible to non-EU students trained here, who are otherwise lost to the system. This could be offset in the form of return-of-service arrangements.
We believe that only by improving working conditions will we see more doctors choosing to stay in Ireland.
We believe that committing to increase the number of consultants in line with the Hanley Report will show we recognise there are too few specialists and we are determined to address this. Irish consultants are well paid in comparison with their international peers. Specialists earned, on average, almost €164,500 in 2014. Irish health professionals are generally well paid by international standards, even when earnings are adjusted for local purchasing power.
We believe, notwithstanding concerns raised by organisations representing consultants, which dispute the accuracy of these figures, that public salaries paid in Ireland represent the higher end of the scale in comparable countries across the world.
Irish consultant salaries continue to be among the highest internationally, despite pay for newly appointed consultants being reduced by 30% in 2012. This pay cut has since been largely reversed. For posts currently open for recruitment, over nine years a Type A consultant’s pay rises from €127,000 to €175,000, a Type B consultant’s pay rises from €120,000 to €157,000, and new entrant Type C consultant’s pay rise from €105,000 to €134,000, respectively.
During the height of the recessionary budgets, with the State facing an unmanageable deficit and unprecedented financial meltdown, Sinn Féin advocated cuts to consultants’ pay and to the pay of other high earners, proposing to use those funds to maintain supports for our most vulnerable children, elderly and sick people.
We do not believe any person of good conscience could question this position.
Budgetary times have moved on. We must now examine the question of consultants’ pay and face the current realities of recruitment and retention.
In recognition of the difficulties encountered by hospitals trying to fill consultant posts in a health system that is under-resourced, understaffed and overloaded, Sinn Féin supports the recent moves by the government to reverse the 30% pay cut for new consultants introduced in 2012.
However, we are convinced that it is the negative work environment that remains the greatest barrier to the recruitment and retention of consultants.
Sinn Féin is determined to recruit 800 additional consultants over five years, with further recruitment to follow during a second term of government.
The particular types of consultants most urgently needed will be identified by the Strategic Medical Workforce Planning (MWP) Project and will cover both adult and paediatric specialties.
This rebalancing of the proportions of consultants to non-consultant hospital doctors (NCHDs) across the workforce will also help to stem the flow of junior doctors from our system, as greater opportunities for training and career progression will be open to them.
Overall, this would lead to a total of 3,600 consultants by the end of the five-year period, taking into account those leaving the system due to retirement.
Guaranteeing that our health service has adequate numbers of consultants (as is the case in other jurisdictions) would in itself make taking up posts here, and indeed remaining in them, more attractive.
There are problems with the amount of private work being done by consultants who are on Type B contracts. HSE director general Tony O’Brien has sent forensic auditors to look at the group that runs St Vincent’s and St Michael’s public hospitals. With respect to the consultants on Type B contracts, the HSE is of the opinion that they are not legally allowed to perform the level of private work currently undertaken.
Sinn Féin believes that the public benefits most from consultants with Type A contracts and we would like to see more fully public contracts.
If there are difficulties with recruiting full-time consultants on Type A contracts, consideration could be given to part-time contracts, but in these cases specialists would only be paid for the hours of public work that they undertake. There would be no subsidy, direct or otherwise, for their private practice, including use of public hospital facilities or extension of indemnity cover (save in the circumstances indicated below).
With this objective in mind, given our determination to eliminate private activity from public hospitals and with the express backing of the public via a clear electoral mandate, we would commence a renegotiation of the Consultants’ Contract 2008.
The new contracts would include protected time for teaching and facilities for research and academic collaborations.
Public consultants could also generate further income by undertaking additional activity transferred to them from the new COMHLIOSTA system outlined in section 1.5.
Certain strategic extensions of indemnity cover may continue to be approved for certain procedures that are disproportionately carried out by the private sector.
Overcrowding in our Emergency Departments (EDs), and more generally across the health service, has long been at crisis levels.
The ‘Trolley Watch’ figures provided by the Irish Nurses and Midwives Organisation (INMO) regularly highlight the impact on the sick and vulnerable of decades of government failure.
The crisis is partly a reflection of inefficiencies within the system – not all hospitals discharge seven days a week, for example. In the main, however, it is directly due to lack of capacity of staff and beds; exit packages, including home help hours and home care packages; nursing home beds; and so on. The situation is worsening, with ‘January-type’ overcrowding now a year-round phenomenon. July 2015, for example, was the worst July ever recorded for overcrowding.
Research on overcrowding in emergency departments consistently shows a direct, negative, correlation between ED waiting and length of inpatient stay and, crucially, with overall outcome. Overcrowding is not just a bad use of resources – it has a direct impact on patient safety and mortality.
Recent data from the OECD Health at a Glance 2014 report show that Ireland is below the EU average for the number of doctors per 1,000 people (Ireland has 2.7, compared to the EU’s 3.4).
The number of hospital beds per 1,000 people is also below the EU average (Ireland has less than 4 compared to the EU’s 5.2). There were 12,683 beds in 2013.
It was identified as far back as 2006 that hospitals here were operating at close to 100% capacity. The OECD report confirms this still to be the case. It should be noted that bed occupancy rates that exceed 85% increase the risk of harm and of hospital-acquired infections.
During 2014, ED performance in terms of trolley waits worsened. In September 2014, the INMO indicated that the number of trolley waits was 6.5% worse than in 2013.
The key causes of delay for patients in EDs are:
What is needed to address these issues?
As the Emergency Department Taskforce reports of 2006 and 2014/15 show, the solutions to the emergency department crisis have not changed. The analysis has been done. The solutions are known and effective, though only when adequately resourced.
However, the reality is that between 2008 and 2013, the governments of Fianna Fáil, Fine Gael and the Labour Party inflicted crippling damage on our health services and more than 1,600 acute hospital beds were lost.
A sustained and sustainable solution to the emergency department crisis will not be achieved without significantly increased investment across the whole system.
While guided by medical evidence, best practice and the fact that quality of care is paramount, Sinn Féin recognises the role of smaller hospitals, not only in the provision of vital health services but in terms of local employment and community identity.
We are committed to ensuring that this role is protected and enhanced. The experience of many communities across Ireland has been one of cuts and broken promises. This must stop.
Hospital staff, patients and communities should be confident that the State values the services provided by smaller hospitals and is committed to a sustained and viable future for them.
The role of each small hospital will, of course, vary depending on local considerations. We need to examine the possibility of expanding certain surgical services and ensuring that specific medical services for chronic conditions, testing and screening are also provided.
The delegation of a range of tasks currently undertaken by Model 4 hospitals, but more appropriately delivered by smaller hospitals, will be essential, thereby allowing larger hospitals to focus on more specialised care. Staffing and funding should follow suit.
Smaller hospitals have developed strong links with primary care and have a further role as rehabilitation facilities. They are well placed to provide a link between Model 4 hospitals and primary care.
The training and rotation of medical staff across larger and smaller hospitals, a hub and spoke model, can ensure that smaller hospitals have permanent access to highly trained and motivated staff.
The waiting list crisis is one of access, of capacity, of funding and of resources.
Despite initiative after initiative, this issue has not gone away and it is worsening.
At the end of July 2015, there were 401,060 people on the list for a hospital outpatient appointment.
| Outpatient appointment waiting list | |
|---|---|
| 0-3 months | 151,141 |
| 3-6 months | 84,786 |
| 6-12 months | 98,508 |
| 12-24 months | 64,006 |
| 24-36 months | 2,146 |
| 36-48 months | 385 |
| 48+ months | 84 |
| Total | 401,060 |
| Longest Outpatient Waiting Lists | |
|---|---|
| ENT | 51,441 |
| Orthopaedics | 50,601 |
| General Surgery | 35,502 |
| Dermatology | 31,909 |
| Ophthalmology | 27,752 |
| Urology | 20,960 |
| General Medicine | 21,845 |
| Gynaecology | 22,656 |
At the end of July 2015, there were 68,786 people waiting for an inpatient/day case appointment.
| Inpatient appointment waiting list | |
|---|---|
| 0-3 months | 26,391 |
| 3-6 months | 16,127 |
| 6-9 months | 9,870 |
| 9-12 months | 7,335 |
| 12+ months | 9,063 |
| Total | 68,786 |
| Longest Inpatient Waiting Lists | |
|---|---|
| Ophthalmology | 11,049 |
| General Surgery | 9,961 |
| Orthopaedics | 9,717 |
| ENT | 6,698 |
| Urology | 6,218 |
Repeated comparisons of healthcare waiting times with other OECD countries show that there is very significant room for improvement in Ireland.
New waiting time targets were introduced by Minister Varadkar in mid-2015. But rather than trying to solve the problem, the minister simply shifted the goalposts, extending the waiting time target from 12 months to 18 months.
As far back as the 2001 health strategy, Quality and Fairness, there was a commitment that “by the end of 2004, no public patient will have to wait for more than three months to commence treatment, following referral from an outpatient department”.
No serious effort was ever made to achieve this target and waiting times have grown since. Former health minister Dr James Reilly set a target of one year to be seen on an outpatient basis and a target of eight months for inpatient or daycase treatment. This target was nearly achieved for a brief period in 2012 but the waiting times have been increasing since.
The fact that the number of people waiting more than 18 months for inpatient or daycase treatment has soared by 7,100% since June 2014, while long waiters on outpatient lists are up 465% for the same period, shows, beyond doubt, that Minister Varadkar’s measures on waiting lists have failed. The ever-lengthening hospital waiting lists are a product of understaffing, a lack of capacity and inefficiencies in the system. During the economic crisis Fine Gael and Labour cut health funding by 20% and cut the number of healthcare staff by 12%.
Scoliosis is a deformity of the spine and there are 174 children waiting for corrective surgical procedures, more than double the number in 2009.
Those waiting are often in pain and have significantly reduced quality of life. The longer the wait, the more the condition worsens, leading to more complex and expensive surgeries. Research suggests a 15%-30% increased cost associated with correcting the more severe curves of the spine.
While the government has acknowledged that the waiting times for spinal surgery services at Our Lady’s Hospital Crumlin, the main site for such operations, are unsatisfactory and while it has allocated funding to appoint an orthopaedic surgeon, anaesthetist and support staff at Crumlin, there has been little improvement in the waiting lists.
We understand that only one of these posts has been filled. Additional recruitment must be prioritised. Capital funding has been agreed for a new theatre site at Crumlin and capacity in other hospitals is being assessed.
As part of our general proposals for additional recruitment, we would appoint an additional orthopaedic surgeon, along with anaesthetist and support staff, until the waiting list is brought down to under three months. When this target is achieved, the new posts can be used to ease the pressure in a more general paediatric orthopaedic role.
These additional 9.5 posts, including a consultant orthopaedic consultant, would cost €742,551 in pay and €400,000 in non-pay costs. Total: €1,142,551
Ireland had the highest birth rate of all 28 EU member states in 2014. Despite this, maternity care has been left in crisis, with shortages of staff in hospitals across the State.
The sector has been traditionally underfunded over the last 20 years and Ireland is lagging behind international standards. This has led to tragedies that include deaths in healthcare settings across the State. Since 2012, four hospitals, Portlaoise, Galway, Sligo and Cavan, have been investigated following deaths and neonatal deaths.
It is evident that there are underlying issues with care. The HSE has failed to have oversight of individual maternity hospitals.
Our maternity services are severely understaffed, lacking both midwives and obstetricians. The INMO says that more than 600 midwives need to be recruited to achieve basic safety levels and it was also shown last year that Ireland has the lowest number of obstetricians per 100,000 women across all OECD countries.
Questions about the best kind of maternity services also need to be addressed. There are benefits and shortcomings with either a fully obstetric-led system or a fully midwife-led system.
We should hold positive maternal and neonatal outcomes as the main goal, but we must also be aware that women at low risk should be offered midwife-led continuity models of care. Expectant mothers must be listened to and placed at the centre of policy.
We must also ensure that unnecessary interventions are avoided. There is a wide variation in Caesarean-section rates across the State, but all of our maternity hospitals show rates that are above the 10%-15% level recommended by the World Health Organisation.
It has been suggested that the high rate of C-sections in the Rotunda is linked to a shortage of delivery units. Surgical interventions are expensive and, when occurring unnecessarily, can cause harm and must be reduced.
As well as funding, however, the system desperately needs humanity. The bereaved must be listened to, treated sensitively and with respect, and given the time they need.
Guidelines on how the remains of loved ones are conveyed to parents and how and where to break bad news for bereaved couples need to be improved.
Logistical issues must also be addressed. In many hospitals the ward for miscarriages/D&C procedures is on the same floor as the post-natal care ward for women and babies. Women who have had a still-born baby can be placed in aftercare wards. Space must be examined and greater sensitivity employed.
Midwives play a pivotal role in the health system. A survey carried out by the INMO highlighted the shocking statistic that no maternity hospital or unit in Ireland had the internationally recommended midwife-to-birth ratio of 1:29.5. The average Irish ratio was found to be 1:38.
In 2014, the number of registered midwives in Ireland was 18,217. However, the number of active midwives was only 11,020.
The public service moratorium has had a severe impact on staffing levels, reducing nursing/midwifery posts from 39,006 in 2009 to 34,914 in 2014.
In 2014, the INMO said that an additional 621 midwives were needed to ensure Ireland was in line with the recommended staffing levels for better care and safety. The average annual cost of employing a whole-time midwife in 2014 was €51,188.
Increased workload and stress, and dissatisfaction with clinical practice, has resulted in many midwives leaving for other areas of nursing, such as public health and education.
Perceptions of poor pay and trends towards reducing working hours and early retirement have also contributed. The lack of adequate workforce planning in the maternity system contributes to workers feeling unprepared for the tasks that they face. Resources are considerably constrained, which also impacts on staff.
A lack of funded posts means that not all newly qualified midwives can find work. Pressure on inexperienced staff can lead some newly qualified midwives to feel unsupported and to consider leaving the profession. Insufficient numbers of experienced midwives mean newly qualified members of staff lack senior support.
In an ageing workforce such as midwifery, staffing shortages must be countered by reassuring graduates that they will work in a system that supports them, allows professional satisfaction and provides time for further training. We must address the environment in which midwives work to ensure that we can retain adequate numbers.
In the past, statistics have grossly inflated the real number of midwives. An INMO presentation to the Oireachtas Health Committee in 2013 showed how figures were misrepresented and made clear the reality for midwives in employment. The INMO pointed out that, “in Ireland, the undergraduate nurse/midwife, when undertaking their rostered placement, is counted as 0.5 of a whole-time post”.
One of the most serious repercussions of the midwife shortage is that it adds to the pressure in neonatal units, which are experiencing an unprecedented workload.
Services in the neonatal unit at Limerick Maternity Hospital were recently curtailed because of the lack of qualified midwives. Low staffing levels in a hospital can also have a knock-on effect in the community, as midwives are pulled in to cover the labour ward.
A What Matters To You? survey in 2014 highlighted the unmet demand for midwives. Just 5.5% of respondents said that they had access to midwifery-led care in their area. Of those that did not have access to the care, 55.5% said that they would avail of midwifery-led care if it was available.
The community midwifery Domino service, similar to that offered by the National Maternity Hospital in Holles Street in Dublin, is a positive example of midwife-led care. For women assessed to be at a low risk this is a way to provide safe, responsive care at less cost to the State.
Analyses have shown that the cost of a normal birth was “€574.30 in the Midwife-Led Unit (MLU) and €631.64 in the Consultant-Led Unit (CLU). MLU births thus cost €57.34, or 10%, less than those in the CLU” (HSE, 2009).
Women in the MLU group had statistically significantly shorter postnatal stays in hospital, with 17% staying only one day, compared with 9% in the CLU. They continued to have postnatal care from the MLU midwives in the community, with an average of 2.04 visits.
Neonatal outcomes in the MLU study showed no statistically significant difference between the two groups, despite the shorter hospital stays for women in the MLU group.
There have been some developments with regard to maternity care services in recent months. The 2015 HSE Service Plan highlights the need to invest in maternity services in Ireland. Maternity staff, patients and the maternity care system have been singled out for mention.
One of the recommendations is to “undertake national maternity service improvements including the appointment of additional staffing in line with HIQA Galway Report recommendations, the implementation of a national model of care for maternity services and the establishment of a national maternity office in the Acute Hospital Division”. (Health Service Executive, 2015)
Women should have the option to avail of midwifery-led care if their pregnancy is defined as low risk. Expectant mothers should be at the heart of the care delivery model.
Opportunities for further professional development should be made available.
Midwives should have the chance to become Specialist Midwife Practitioners in fields such as diabetics, cardiology, haematology and bereavement. Training in ultrasonography should also be offered and this would also facilitate the rollout of a 20-week scan to all pregnant women as standard.
These measures could enhance the attractiveness of the profession and aid in the retention of midwives.
Nursing and midwifery graduates who qualified in 2009 started on the second point of the salary scale, which was €33,470. Posts currently vacant are being advertised at a starting salary of €27,211. This represents a cut of €6,259.
We recognise that the Lansdowne Road Agreement will have some positive effect for this grade of worker.
The community and domino midwife scheme operating in the National Maternity Hospital, Holles Street, and in three other hospitals, involves midwives rotating through the labour ward to ensure their skills are maintained.
It offers a model of maternity service delivery which should be extended as a major component of the very significant recruitment of additional staff Sinn Féin is proposing.
Sinn Féin supports the planned co-location of the Dublin maternity hospitals with acute adult hospitals. This is necessary and will ensure access to vital specialist services for mothers and babies as required. It has been recommended since 2008 that all maternity hospitals be co-located with adult acute services in order to provide optimal clinical outcomes, and this is reflected in models internationally.
Mental health is an area in which successive governments have struggled to provide an adequate level of service. This is despite the fact that 644,000 people, one in seven adults, have experienced a mental health difficulty in the last year. Moreover, the number of suicides has remained high, with between 495 and 554 deaths per year from 2009-2012.
The funding allocated to mental health is insufficient. The overarching framework document for this sector, ‘A Vision for Change’, proposed a mental health funding target of 10% of the overall health budget. While there have been attempts made to reconfigure health spending in order to afford mental health greater priority, we continue to see funds earmarked for mental health diverted to other areas. Nine years on from the publication of the strategy, just 6% of the total health budget went to mental health, compared to 7.2% in 2006. In 2015, it is predicted to account for just 6.5%. To reach the budget target of 10% would require an estimated increase of €400 million.
Staffing numbers in the mental health sector are likewise, and consequently, insufficient. There are approximately 1,200 fewer mental health staff now than there were in 2006. A report published in June 2015 indicated that staffing numbers were just 77% of the level recommended by A Vision for Change; in Child and Adolescent Mental Health Services (CAMHS) the situation is more severe, with just over half of the staff required in place.
The proposals contained in ‘A Vision for Change’ are sound, but they have never been fully introduced and so-called ring-fenced funding has, in some cases, not materialised. ‘A Vision for Change’ was published in January 2006 and was originally supposed to be reviewed after seven years. This is only occurring now.
Sinn Féin believes that the recommendations of ‘A Vision for Change’ still need to be implemented. In line with this, we would allocate an additional €35 million to be directed towards community mental health services in year one. This will aim to address staffing shortfalls, with a particular focus on staffing CAMHS and ensuring that every area of the state has access to 24/7 crisis intervention services.
The new strategy for suicide prevention, ‘Connecting for Life’, also needs to be incorporated. This sets a target to reduce suicide and self-harm by 10% over the next five years (based on WHO targets). We must also ensure that the numbers of charities working in the area are assessed, and a plan put in place to accredit them, ensuring that work is not duplicated and that they are of a high standard across the State.
Sinn Féin recognises the merits of the Suicide Prevention Authority proposed by the suicide prevention charity, 3Ts, and is favourably disposed to the establishment of such an overarching body on an all-Ireland basis to lead the way and set the standards for all who are involved in suicide prevention initiatives.
We want to see a society in which all citizens, including those with disabilities, can play a full and independent part in all aspects of life, relying, as far as possible, on mainstream services for health, education and employment but with the support of tailored disability services where necessary.
The last Census found that 565,000 people in this State reported having various forms of disability. As these individuals have families, friends and neighbours, disability is something with which we are all familiar, in one form or another.
Disability is a societal issue, affecting people of all ages and their families, directly and indirectly. Three-quarters of those who use disability services are not satisfied with the level of control they have over their lives and those with disabilities have among the highest levels of consistent poverty. People out of work due to illness or disability are five times as likely to be at risk of poverty and survive on the lowest annual average disposable income, compared to other socio-economic groups.
| Disability Services Total Budget | |
|---|---|
| 2012 | €1,554m |
| 2013 | €1,535m |
| 2014 | €1,429m |
| 2015 | €1,459m |
The budget for disability services has been reduced by €95 million since 2012 and by €159.4 million, or 9.4%, since 2008.
There were 21,821 people waiting for speech and language assessments and therapy in April 2015, with more than 15,300 people waiting for assessment by an occupational therapist. Almost 30,000 people were waiting for a physiotherapy assessment.
The government has clearly chosen not to prioritise services for those with disabilities.
Disability service providers have seen their funding significantly depleted over years of austerity budgets. The cuts imposed have gone far beyond efficiencies and have severely curtailed frontline delivery of essential services. Funding for this sector must be increased, and excessively high pay at the top of organisations that provide public services to people with disabilities on behalf of the State can no longer be tolerated.
We must also engage those with disabilities on an individual basis to find out exactly what they need and want. Maximising independence relies on a holistic approach, providing assistance when needed and in such ways that support independence.
In the development of State programmes of support for persons with disabilities, Sinn Féin in government would consult fully with those impacted and the organisations representing them.
We need to move the focus from congregated settings to the community, and not just to smaller and smaller settings but to full integration. Congregated settings are ones where residents live in an isolated institution and are inappropriate homes for anyone, particularly those with complex needs. The focus needs to shift from centre-based services to supported mainstream integration.
The focus must be on empowering the service users to take as full a role as possible. Resources are also needed to support families.
The Health Service Executive has submitted a costed plan to the Department of Health that would see €250 million spent on progressing de-congregation, to ensure that service users live and are supported in community-based facilities. Sinn Féin would allocate the necessary funding.
We must tackle many of the physical, financial and societal barriers that challenge people with disabilities. The personal assistant (PA) system was started by a group who wanted to overcome physical and sensory impairments. The service users were leaders, in that they controlled and directed the help that they would receive to best suit their needs.
However, the quality of empowerment and control by leaders over their service has been eroded, in part due to cutbacks. Sinn Féin would increase PA hours by an additional 500,000 hours each year for three years, at an estimated additional cost of €11.75 million in the first full year, rising to €32.25 million in the third.
The potential loss of the medical card is an immensely significant barrier preventing people with disabilities and chronic illness entering employment. It has also been suggested by advocates working in the field that some people with disabilities, fearful they might lose their medical card, have left employment.
Everybody with serious medical needs should have a secure medical card. Unless the medical card system is reformed, this will continue to act as one of the most significant poverty traps. Sinn Féin would make significant reforms to the medical card scheme, as outlined in section 1.2.1.
The HSE’s Progressing Disability Services for Children & Young People (0-18 years) (PDSCYP) programme aims to deliver health services to those with disabilities in a uniform way, regardless of age, location or disability.
Gaps in provision of services for children and adults have been identified across the State, but the Department has been either reluctant or unable to release this information. €4 million for an additional 80 posts was provided under PDSCYP in 2014, and a €6 million allocation was announced in 2015 for 120 new staff appointments. This is grossly inadequate and in many cases has not even seen provision return to the levels of 2009/10.
The under-capacity of the public system means that parents are forced to spend hundreds of euro every month on private therapy if they want to see their child talk, walk, or have any hope of realising their individual potential. €60 for 30 minutes is a standard price for private Speech and Language Therapy.
Monthly reports under the Disability Act 2005 suggest that priority should be given to Speech and Language Therapy (SLT) posts, then Occupational Therapy (OT) posts and Physiotherapy (PT) posts. Sinn Féin’s aim would be to increase the number of SLTs by 250, OTs by 100, PTs by 100 and psychologists by 150 over our term in government, at an estimated cost of €30.725 million.
There has been little progress on the disability strategy implementation plan, published in July 2013, and indeed the cuts to the overall health budget have undermined many of the worthwhile aims of the strategy.
Timelines are also not strict enough and targets are lacking, with little cooperation across departments.
Action is required across a range of departments and this should be centrally coordinated and driven by the Department of An Taoiseach.
Accountable, high-level responsibility must be assigned to progressively realise the objectives of:
Recognising the importance of Irish Sign Language to the Irish Deaf Community, their families and friends, Sinn Féin supports the granting of official recognition to Irish Sign Language (ISL), thereby affording deaf and hearing impaired users of ISL greater opportunities in a more equal society.
Acquired Brain Injury (ABI) can be defined as any brain injury that occurs with rapid-onset and includes trauma and strokes. There are an estimated 10,000 people per year with an ABI in Ireland. We must help those with neuro-rehabilitation needs to lead full and meaningful lives by giving them quality, tailored rehabilitation and support.
We know that early intervention ultimately reduces the care needed and many studies also clearly demonstrate significant cost-savings post-rehabilitation.
We are currently failing to intervene early enough, as shown by the fact that there are approximately 190 patients awaiting admission to the National Rehabilitation Hospital (NRH). The NRH is currently the only service provider. With 110 beds, it provides complex specialist rehabilitation services, including 56 beds for those with acquired brain injury.
The average waiting time for those with neurological conditions resulting in the most significant impairment is 48.5 days. Specialist paediatric rehabilitation services also have 40 children on the waiting list for the programme, with some waiting in excess of six months.
The National Policy and Strategy for the Provision of Neuro-Rehabilitation Services in Ireland 2011- 2015 needs a meaningful implementation plan based on accurate figures. We need the further development of community-based neuro-rehabilitation teams to provide moderate and high-intensity neuro-rehabilitation in community settings.
Each HSE region, through a mapping exercise, should determine what is needed and reconfigure resources to make up the teams. Evidence tells us that these teams can provide models of care that surpass conventional hospital-based services in economic efficiency and achieve higher levels of patient satisfaction.
Community neuro-rehabilitation teams cost €930,000 per annum. Acquired Brain Injury Ireland has estimated that approximately 12 teams are needed.
Transitional service, an intensive rehabilitation service post-acute injury, is needed to enable people to return home, and costs in the region of €624,000 per annum to operate. At present, there is only one dedicated ABI transitional unit. Three more such transitional services have been identified as needed across the State.
A greater emphasis on community-based care has the potential to reduce the number of older people requiring nursing home care, but this has not been quantified because, as the Department of Health report on the Nursing Homes Support Scheme (NHSS) makes clear, the further development of community-based care is only aspirational.
We estimate that as many as 13% of nursing home residents, possibly as high as the 30% figure given by Alone, would be able to stay at home if the appropriate services were put in place.
Sinn Féin is committed to the provision of healthcare services and social care services as a right, with equal access for all based on need and to the greatest extent that resources allow. This right is especially relevant for older people and the provision of support for older people is becoming increasingly important as our population ages.
We should see improved health and longevity as an opportunity as well as a challenge, with older people contributing to our society. In the words of the Democratic Programme of the First Dáil Éireann, we are committed to the care and support of Ireland’s older people “who shall not be regarded as a burden, but rather entitled to the Nation’s gratitude and consideration”.
People should also have the right to choose how best they will be supported as they age. In the development of State programmes of support for older people, Sinn Féin in government will consult fully with organisations representing older people and with the wider public.
The current State policy of care for older people is based on two pillars: firstly, financial support for nursing home residence; and secondly, the provision of home help, home care and day care for older people living in their own homes.
While most care is provided for people living in their own homes, the bulk of State spending is on nursing homes. In 2015, €315 million was allocated for home help and home care, compared to €933 million for nursing home support.
The vast majority of older people prefer to live out their lives in their own homes if at all possible. Current government policy is supposedly oriented in this direction, but it has failed in practice. Cuts to home help, home care, housing adaptation grants, carers’ supports, and other services have resulted in more people than necessary going into long-term residential care.
It has been estimated that possibly up to a third of people in nursing homes could be at home if adequate supports were provided.
Sinn Féin will enhance home support services as part of a comprehensive programme of reform, with emphasis on the home and the community.
We will tackle the race to the bottom, which has resulted in a serious deterioration in the pay, terms and conditions of those workers and carers who provide care for older people, at home, in the community and in residential settings.
While it has been suggested that the NHSS should be extended to include home supports, this scheme was designed specifically for long-term residential care.
Currently home supports, though inadequate and under-funded, are provided free of charge based on an assessment of need. Sinn Féin believes that they should continue to be provided on that basis. We will develop and implement the recommendations for ‘Reorientation of the Social Care System’ in the Department of Health’s 2015 Review of the Nursing Home Support Scheme.
The implementation of these recommendations will require new and imaginative approaches. For example, collaboration between the Department of Health and the Department of Environment, Community and Local Government is recommended to provide appropriately supported sheltered housing for older people.
Sinn Féin will develop this proposal fully as part of our programme to address the need both for enhanced care and for appropriate community housing for older people, especially in the context of the wider housing crisis.
Most older people requiring care and assistance with daily living are looked after by unpaid family or friends in their homes. Therefore, it is vital that the role of carers is fully recognised and that current State supports for carers are enhanced. Sinn Féin opposed the cut of €325 that was made by the government to the Respite Care Grant and provided for its restoration in each of our annual Alternative Budgets.
Respite care involves giving families and carers help in caring for their loved one for a short period. This care is provided by the HSE and by voluntary organisations. Current provision is far short of what is needed. Without adequate respite, family carers are themselves left more vulnerable to ill-health. Sinn Féin would increase respite care service provision for older people by 20%, at an estimated cost of €6.24 million.
Given their great commitment and experience, it is also important that carers are consulted in the development of government policy and in the necessary reform and enhancement of State programmes for elder care. Sinn Féin will ensure such full consultation.
Even with greatly enhanced home and community care for older people, many will still require long-term residential care and the numbers of people in nursing homes will grow with the ageing population. It is essential that people are supported in long-term residential care and that the highest standards are maintained.
The Nursing Home Support Scheme (NHSS ‘Fair Deal’) is the basis of State support for long-term residential care for older people. It is jointly funded by contributions from nursing home residents based on their means and a State contribution based on cost of care. (The average ratio of personal and State contributions is roughly 1:3).
The NHSS currently costs the State around a billion euros per year and the cost is set to increase with growing numbers of people requiring nursing home care, from 24,000 in 2015 to more than 33,000 by 2024.
Sinn Féin commits to, in tandem with increasing community services and thereby reducing demand, funding an additional 900 beds in year one, a further 800 additional beds in year 2, and 700 additional beds in year 3 and thereafter. This would require an estimated budget increase of €125.4 million by year five.
Given the growing need for long-term residential care, Sinn Féin believes that the current overreliance on the private nursing home sector to provide the beds required in the years ahead is not sustainable. The trend in recent years for the HSE to close public nursing home beds should be reversed.
During the ‘Celtic Tiger’, the need for more nursing home beds was addressed not in a comprehensive care-based and person-centred way but on the basis of property development tax incentives. Nursing homes sprang up and in some cases, standards of care came second to the profit motive.
The Department of Health’s 2015 Review of the NHSS states that “the need for further incentivisation for further investment in the sector is currently being evaluated”. Any evaluation must learn from the mistakes of the past and not repeat them. Care must be the priority.
The nursing home sector should be developed in tandem with community- and home-based care. There is a role here for the Department of Health, the Department of the Environment, Community and Local Government and for the local authorities in developing innovative forms of housing and long-term residential care.
This will require careful planning and coordination and to this end Sinn Féin will establish an inter- departmental and inter-agency Working Group on Community and Residential Care for Older People.
The provision of health and social care services for people with dementia has become an increasingly important issue. That is set to continue with our ageing population, longer life expectancy and the expected trebling of the numbers with dementia over the coming years. Yet health and social care services do not match up with need and are often inconsistently provided, if provided at all.
It is estimated that there are 48,000 people living with dementia in this State, 63% of them residing in their own homes.
Chronic disease represents the bulk of the workload of our hospitals and incidences are predicted to rise. The long-term care of patients with conditions such as asthma, diabetes, and heart conditions represents a significant unnecessary cost burden on our acute hospital services, when more timely and appropriate care can be provided at the primary care setting.
While some measures on management of asthma and diabetes were announced in the most recent GP deals, they are very limited, allowing for just two years of asthma and diabetes care and only to those already receiving a certain level of care.
The Cycle of Care in General Practice for GMS patients with Type 2 Diabetes is set to commence before the end of 2015, with approximately 70,000 medical card-holding patients expected to benefit. It is estimated to cost €4.5 million in 2016. This will lead to the development of a register of those with Type 2 Diabetes and provide for two structured visits per year.
It is essential that this rollout should entail not just paying GPs for this care but providing patients with rapid access to endocrinology outpatient departments, diabetic nurses and ophthalmological review.
The number of consultant endocrinologists, diabetic nurse specialists, and ophthalmologists must be increased as part of the overall investment in increased capacity across the health system. This is addressed in section 2.3 on medical consultant recruitment.
Separately, the Heart Watch scheme is an example of considerable success in chronic disease management. This is a GP scheme focusing on secondary prevention for patients who have experienced a serious heart event or had significant cardiovascular disease. It reduced five-year mortality to 5%, compared to almost 15% for those not on the scheme.
Unfortunately, only 20% of GP practices were involved in the programme, even though State-wide rollout was promised. This scheme needs to be further resourced and rolled out across the State. We would provide an additional €4.5 million for this scheme in year one.
Furthermore, in relation to the management of asthma, the first step of the HSE National Clinical Programme for Asthma should be funded. This has been estimated by the Asthma Society of Ireland to cost approximately €2.5 million.
Currently, one person dies from asthma every week. Additional funding for primary care will provide a free annual asthma review and a written asthma action plan for all people with asthma.
Coeliac Disease is an auto-immune disease affecting approximately 46,000 people. If a person with coeliac disease eats gluten, the lining of the small intestine becomes damaged. The treatment is adherence to a gluten-free diet. If the condition is not diagnosed or if diagnosis is delayed and treatment not initiated, it can result in serious complications, including osteoporosis and cancer. If coeliac disease exists in a family there is a one in ten chance of other members of the family developing the condition, yet we have no screening programme. In keeping with international guidance, Sinn Féin proposes to offer serological (blood) testing to first-degree relatives of people with coeliac disease.
Building adequate capacity across our health system and eliminating the unequal barriers to access requires significant and sustained public investment.
Saving our health system from the potentially permanent emigration of our trained medical professionals in all fields requires a long-term and credible commitment from the public and its elected representatives. This requires a commitment not only to the ideal of transforming our health system into one that provides both first-class care and a caring work environment but also a commitment to raise the revenue required to achieve this. The only credible solution to our health crisis is one with sustainable funding attached.
The task of putting a figure on how much additional funding is required to provide a first-class and universal system is not an easy one. We have endeavoured throughout this document to develop evidence-based costings but it must be noted that the outcome of negotiations on public sector pay and with the pharmaceutical industry would impact greatly on the cost of individual measures into the future.
Our costing development work was further frustrated by the staggering deficit of data held centrally by either the Department of Health or the HSE. On a number of occasions, they simply would not, or could not, provide basic data required to determine what we are currently delivering for our public spend. This in itself is of serious concern.
It is undeniable that our public health system continues to suffer acute and chronic underfunding. The annual deficits run up across the system every year, alongside lengthening waiting lists and numbers of patients on trolleys, are a testament to the failure of successive governments to allocate adequate funds.
A deficit of circa €600 million is anticipated by the end of 2015. For some commentators, including recently the government’s Irish Fiscal Advisory Council, these continued health spending overruns constitute a looming crisis. For Sinn Féin, the hundreds of thousands of people who are left without timely access to the healthcare they need, despite these overruns, is the very real and present crisis.
Sinn Féin is committed to investing what it takes to deliver our vision for the health of the Irish people. And it is possible, despite the aforementioned obstacles, to estimate the additional funds that will be required in the years ahead by examining the macro domestic and international picture.
At 8.1% of GDP (this figure relates to 2012, which is the most recent year available from the OECD) our total expenditure on health as a portion of GDP is lower than the OECD average of 8.9%. However, our overall per capita spend, the sum of state-spending and private spending, at $3,663 is higher than the OECD average of $3,453. And this is despite our comparatively younger population.
Yet we do not see any benefit from this, with lower numbers of doctors and hospital beds per resident than our European neighbours, as was acknowledged by the European Commission in its 2015 Country Report. This is likely because the proportion of our total health spend that comes from private spending by members of the public (including out-of-pocket spending and private health insurance) relative to public spending is greater than average – and significantly so in the case of countries with the type of health systems we should aspire to build.
Public expenditure accounts for just 68.5% of our total spending on health, compared to an OECD average of 72.7 %, with 78.7% in France, 84.1% in Sweden, 85 % in Norway and 86.6 % in Britain (OECD Health at a Glance 2015).
This suggests that we are channelling our money the wrong way. The current proportions in the spread of health funding across public spending, private health insurance and out-of-pocket charges (the money spent by individuals on healthcare, including GP care and charges for medicines) drives inefficiency – as a nation we are literally getting less for more.
The current heavy reliance on private health insurance and out-of-pocket charges is also an inherently regressive policy choice.
For individuals earning a wage of €17,000, €35,000, and €65,000, respectively, having to pay €144 out of pocket for drugs (which is the maximum monthly spend on drugs before the Drugs Payment Scheme kicks in) accounts for 10%, 5% and less than 3% of their respective incomes. Likewise, having to purchase an average private health insurance premium at €1,200 takes up 7%, 3.4% and 1.8% of low-, middle- and high-income groups’ income, respectively.
A leading health economist, Professor Charles Normand, has argued that it is possible to deliver universal healthcare without necessarily changing the share of Gross National Income accounted for by our total expenditure (public and private) on healthcare. He suggests that efficiency gains of 2% a year and a 2%-3% growth in revenues from wider economic progress would also be sufficient to accommodate demographic pressures. However, healthcare still needs to be funded and delivered differently to achieve this. The spread of funding across public spending and private spending by the public, i.e. out-of-pocket charges and private health insurance, must also change.
Normand suggests that because the money spent on health ultimately comes from households, the question for policy makers to address is this: what is the optimal way for the money to get from these households to the healthcare provider?
In Sinn Féin’s view, the most effective, equitable, and efficient way to do this is through progressive taxation and adequate PRSI contributions.
Private health insurance contributes significantly less in value than it does in cash to the health system. Transaction costs vary widely across health systems, from levels as low as 7%-8% in tax- funded systems to up to 30% in complex mixed models such as that in the United States.
In 2012, the year for which the most recent figures are available, public spending on health was €14.1 billion and private spending by the members of public was €4.7 billion, bringing total spending on health to €18.8 billion. Of this, private health insurance accounts for €1.9 billion, out-of-pocket expenditure amounts to €2.45 billion and private sector capital expenditure €300 million.
By progressively re-channelling private spending by members of the public into public spending and through better stewarding of spending, we can achieve much greater efficiency and fairness. We can deliver more with the same.
The Fine Gael and Labour Party Government proposed to introduce Universal Private Health Insurance (UHI) as the new funding model for health.
It was entirely foreseeable that health costs would rocket and disadvantage for people with disabilities and chronic illness would worsen as an inevitable result of the role envisioned by government for multiple private insurance companies. The government’s model also missed out on the benefits of a single purchaser.
Sinn Féin consistently called for UHI to be shelved. UHI, previously the government’s flagship health policy, would have seen all members of the public forced to buy health insurance. When introduced in other countries, it has led to a reduction in services and increases in costs.
The Department of Public Expenditure (DPER) raised “fundamental concerns” about UHI. It appears that those less well-off would have no guarantee to services or medications for minimum cost. This means that those currently covered by medical cards and long-term illness cards in particular would lose out under the proposed system.
DPER even raised the possibility of the system running out of money before year end. The Society of Actuaries in Ireland also warned that insurers could need up to €2.4 billion in additional regulatory capital to operate UHI. How could taking money away from patient care and handing it to private health interests benefit our health system?
We also do not know what they intended to cover in the ‘basket of services’. The Irish Medical Organisation predicted that “the system as outlined will restrict choice and lead to rapid closures of smaller health facilities throughout the country”.
Sinn Féin is strongly opposed to the for-profit slant of Fine Gael’s approach to healthcare. UHI represented a fillip for private health insurance companies and for-profit healthcare companies. Similar models in the Netherlands have seen the quality and range of care continually reduced, with premiums rising by up to 40%. Furthermore, the majority of the population find they have to purchase additional insurance cover to make up the shortfall in UHI.
We also see in the United States that the system of privatisation simply diverts badly needed funds away from frontline services towards administration and introduces the forces of the market economy, with “consumers” buying “products”. The multi-payer model also requires a great deal of regulation, again taking the focus away from treating patients.
The publication of the ESRI Report ‘An Examination of the Potential Costs of Universal Health Insurance in Ireland’ put a long overdue final nail in the coffin of the government’s plan.
When Fine Gael and Labour should have been using their years in office to pursue a system of universal healthcare that would allow timely access to suitable care, free at the point of delivery for all citizens, they simply looked to Universal Health Insurance as a solution for everything. In reality it was merely a funding model, and a fundamentally flawed one at that.
Fianna Fáil are content to leave things exactly as they are. Their recent health policy name-checked every lobby group but failed to challenge the structural inequality at the heart of our two-tier health system or to explain how they would pay for it all.
They failed to challenge this inequality because they are ideologically wedded to the current system, where ability to pay trumps medical need. Fianna Fáil may, as their health policy document states, “believe that any extra money that becomes available should be used in developing and maintaining services”, but Sinn Féin does not believe hoping the money will turn up is a coherent approach to healthcare funding. The sort of investment that our crisis-ridden health system requires doesn’t randomly become available.
Sinn Féin is proposing a new funding model for health, a model in which public expenditure makes up a far greater portion of the total spend on health than it does at present.
Public investment in health from existing sources must rise by 2%-3% per annum to accommodate demographic pressures on our health system. In addition to this, Sinn Féin proposes to increase public spending on healthcare by an additional €3.3 billion over the next five years, beginning with €794 million in year one. The Department of Finance figures for the period 2017 to 2021 set out a combined net fiscal space of €8.6 billion. In prioritising significant and targeted investment in the health service, Sinn Féin will allocate €3.3 billion for health from the overall fiscal space. During a second term of government we would continue with year on year increases to spending reaching €5 billion.
The subsidisation of the private health system at the expense of public healthcare must be ended. Cancelling the relief on private health insurance, which is a tax expenditure that disproportionately benefits the better off and facilitates queue skipping, would free up €355 million to be spent for the benefit of everybody. This is a conservative estimate, given that it is based on 2014 figures.
The HSE has estimated that the private health insurance market generates approximately €500 million per annum for public hospitals. In order to end the unfair differentiation between public and private patients in these hospitals, it is vital that this revenue stream be replaced. As part of that process, and as discussed in section 1.5, the €355 million tax expenditure that currently subsidises private health insurance should be rechannelled into the direct funding of the public hospitals, along with the elimination of private activity from these sites.
People would be better off under Sinn Féin’s funding model, not only in terms of the tangible benefits for their health, but in their pockets also. Medical card holders would save up to €25 per month from the abolition of prescription charges and everybody else will save up to €144 per month from the introduction of free prescription drugs. Non-medical card holders will save €100 per A&E visit and up to €750 per year of inpatient charges. Annually expanding numbers will save €50-€60 per GP visit with free GP care for all reached in the second term of government. Up to 45% of the population will save an average of €1,200 on private health insurance premiums they are currently paying out of fear, as we transform the public health system into the system of choice.
We must become better stewards of our health spending. This is not about pursuing efficiencies in order to facilitate cuts to the overall health budget. Rather, it is about ensuring we deliver the best care possible from the funds available.
A moratorium on recruitment across all areas of the public sector was introduced in March 2009. It created a health system propped up by agency staff on salaries many times that of permanent staff. Certain agency doctors can cost a hospital approximately €1,000 a day. In one year alone, 50 agency doctors each earned approximately €300,000.
Launching their pre-Budget submission for 2016, the Irish Hospital Consultants Association made the case that an agency consultant is twice the price of a long-serving permanent consultant and three times the price of a new consultant.
According to the HSE Performance Report for the month of January 2015, it spent €27 million on agency staff. In January 2013 it had spent €19 million.
We need to ensure that the HSE reduces reliance on agency staff and makes permanent posts attractive for qualified applicants. The current approach is clearly costing us dearly, and not just financially.
Continuity of care is also undermined when there is an overreliance on agency staff who are, by their nature, often employed only for short periods. While the greater number of agency staff are competent and committed healthcare providers, if issues do arise they can be harder to monitor if staff are moving across facilities.
Earlier in 2015, we heard reports relating to concerns about locums in radiology, where it was suggested that at least one patient had had a delayed diagnosis of cancer. Dependence on agency staff must be greatly reduced. Sinn Féin’s recruitment proposals outlined in Part 2 – Capacity of this document would achieve this.
The State drugs bill in 2014 was €1.702 billion (€1.253 billion General Medical Services Scheme – €470 million Community Drug Schemes).
It is well documented that the cost of on-patent and off-patent drugs in Ireland remains very high by international standards.
While the government and HSE claim that the average price of medicines on each of the State drugs schemes has reduced since 2000 thanks to the various measures introduced, others, including Sinn Féin, contend that much more needs to be done.
We are not alone. The European Commission’s December 2012 winter review, as part of the Troika’s quarterly monitoring of Ireland, stated:
“While all EU countries have seen substantial increases in drug costs since the turn of the century, Ireland’s increases have been among the sharpest, nearly tripling from 2000 to 2008. In 2010, per capita spending on pharmaceuticals in Ireland was the highest in the EU, 34% above the average, while outcomes are not better than the average for EU countries over a range of health indicators. This suggests a potential for savings well beyond the measures already announced.”
A 2013 report from the ESRI said that in 2010, Ireland was the third most expensive place for drugs out of 25 OECD member states. Using 2013 data from the same report, the ESRI found in-patent and generic pharmaceutical prices were higher in Ireland, while acknowledging lower off-patent pharmaceutical prices in Ireland.
The formula employed to calculate the cost of on-patent medicines is agreed with the Irish Pharmaceutical Healthcare Association (IPHA). The price paid in Ireland for a particular medicine is referenced against the average price of a basket of nine EU countries.
The ESRI, in their ‘Pharmaceuticals Delivery in Ireland - Getting a Bigger Bang for the Buck’ report, stated that significant savings, in the region of 25%, could be achieved by using the ‘lowest’ rather than ‘average’ of the nine countries.
IPHA Chief Executive Oliver O’Connor acknowledged that “overall, Irish prices are still 15%-25% higher... than the EU average”. Opposing voices, in particular the major pharmaceutical companies, which contend that this cannot be done because of the risk to pharmaceutical industry jobs, must be challenged.
Sinn Féin has long identified the need for an improved deal for the Irish taxpayer.
So far, savings have been made by the HSE by switching to a greater proportion of generic drugs; reference pricing, which allows swapping for cheaper drugs; and successive deals agreed with the IPHA.
The State will contend that the HSE has been successful in providing access to many new medicines, whilst at the same time reducing prices of new and existing medicines.
They will say they have delivered savings of €1.5 billion between 2006 and 2013, with a further €400 million in the current agreement (these figures are strongly contested) and that a significant proportion of this (between €210 million to €250 million) will be reinvested in new medicines. They will say expenditure on reimbursed items has remained stable between 2009 and 2014, despite the introduction of a range of expensive medicines.
However, the undeniable fact is that the Irish taxpayer is still paying too much for on-patent medicines by international standards (1.8% ahead of EU9) and, importantly, our system still uses far too much of them. On-patent drugs account for 78% of the State’s public health drug budget. The most recent IPHA Agreement, which deals with on-patent drugs and off-patent drugs that do not have a generic equivalent, came into effect on 1 November 2012. Future agreements must deliver a better deal for the Irish taxpayer.
The current formula means that when a company applies for reimbursement of a new patented medicine, the maximum price that it can apply for is the average of the approved prices across the nine EU member states detailed in the most recent (2012) IPHA agreement. The nine countries are: Belgium, Austria, Denmark, Finland, France, Germany, Netherlands, Spain and Britain.
Sinn Féin would seek to move away from this methodology, as we firmly believe that doing so provides scope for considerable savings.
The 2012 agreement also requires that companies would submit a dossier of economic and clinical data in support of reimbursement at the price applied for. This is assessed by the National Centre for Pharmacoeconomics, which is based at St. James’s Hospital, and in the case of exceptionally high-cost drugs, by the National Drugs Committee.
Specifically, the Health Act of 2014 requires the HSE to consider:
The increased use of off-patent and generic medicines presents massive potential savings. It is very clear that the State and consumers pay far too much for generic medicines (22% above EU9 basket) and are using far too few of them.
The State would argue that there have been significant savings in the price of off-patent drugs (branded and generic) under negotiated agreements, the most recent being with the Association of Pharmaceutical Manufacturers of Ireland (APMI) in May 2014.
At launch, generics are now required to be 60% lower than the pre-patent expiry price of the brand. Sinn Féin believes there is scope to reduce this price further.
The Health (Pricing and Supply of Medical Goods) Act 2013 provides for reference pricing and generic substitution. The Health Products Regulatory Agency (HPRA) has the authority to designate medicines as interchangeable. Interchangeable medicines can then be reference priced.
By 31 January 2015, there were reference prices for 110 groups across 37 different medicines/ combinations. The HSE is reimbursing in the order of 1.5 million claimed items per month for reference-priced medicines. Industry argues that the prices are too low; others argue that they are too high.
The HSE says that they are reasonable and commensurate with continuity of supply and avoidance of co-payments.
The HSE also says that savings of €47.4 million were achieved in 2014 from reference pricing alone and the full-year impact of those savings will be €60 million. They expect a further €25 million saving in 2015. In the off-patent market, generics accounted for 68% of reimbursed claims (by volume) in Q4 2014 and 57% by value. This is far too low.
The establishment of the Healthcare Enterprise Alliance has the potential to play a positive role in the effort to maximise the use of generic and biosimilar medicines.
There remains very considerable scope to increase the amount of generics and biosimilars further. A more vigorous implementation of the provisions of the Health (Pricing and Supply of Medical Goods) Act 2013 would go some way to achieving this.
The HSE Medicines Management Programme was established in January 2013, with the purpose of improving the safe and cost-effective administration of drugs. A series of prescribing meetings were held across the State encouraging the use of generics. This work was done in conjunction with the Irish College of General Practitioners.
Under a current proposal, drawn up by Professor Michael Barry, head of the National Centre for Pharmacoeconomics, GPs stand to gain thousands of euro (approximately €10,000 per annum) in practice supports if they meet certain prescribing targets. Sinn Féin supports the proposal.
If the value of health budgets is to be protected into the future, then action must be taken to guard against potentially harmful, unnecessary interventions and over-treatment. The Institute of Medicine in the United States has estimated that 30% of spending on health is “wasteful and does not add value to the care of patients”. (Canadian Medical Association Journal, 2014)
This is not to suggest that such a percentage would carry over to the Irish context. Health spending in the United States is remarkably high due to the dominant role of private providers and private insurance companies, but the example suggests the impact on scarce resources of unnecessary spending.
‘Choosing Wisely’ campaigns have been initiated in a number of countries, including the United States, Canada and most recently Britain, with a view to minimising unnecessary medical interventions and treatment.
As described in the Canadian Medical Association Journal in March 2014:
“Choosing Wisely Canada is a campaign designed to help physicians and patients engage in conversations about unnecessary tests, treatments and procedures, and supports physicians’ efforts to help patients make smart and effective choices to ensure high quality care.”
It involves tasking the post-graduate medical training bodies and specialist associations with each identifying a list of “five things physicians and patients should question based on evidence of overuse, waste and potential harm”.
Resulting guidance is filtered through to the academic institutions, medical students, physicians and public in the form of “Avoid” guidelines, patient information leaflets on why certain tests and procedures may not be needed and Web resources to aid and facilitate engagements between doctors and their patients.